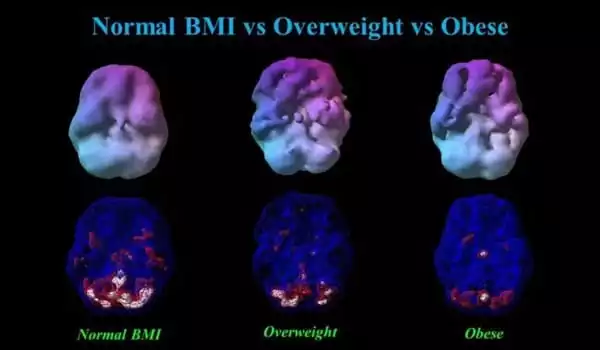
Obesity is linked to an increased risk of cardiovascular diseases, such as diabetes, hypertension, and stroke. These cardiovascular diseases raise the risk of cognitive decline and dementia, but it is unknown whether these factors, particularly obesity and Type II diabetes, are linked to specific patterns of brain atrophy.
Obesity risk factors from one’s family history are linked to changes in brain function, according to a study conducted at Finland’s Turku PET Centre. The findings show that the function of neural networks that regulate satiety and appetite is altered even before a person becomes obese.
Obesity is a growing global health issue, and new interventions to prevent and treat obesity are required. Obesity has been linked to changes in insulin sensitivity and neurotransmitter function in the brain. These changes could account for increased appetite and overeating.
“However, it has not been determined whether these changes are visible in the brain before a person develops obesity and if these changes would increase the risk for future obesity,” says Doctoral Candidate Tatu Kantonen of the University of Turku’s Department of Clinical Medicine.
Disturbance in the neural networks controlling satiation and appetite can thus be seen before a person develops obesity, and these brain changes are linked to family-related obesity risk factors. The findings may have implications for the development of obesity prevention and treatment interventions.
Tatu Kantonen
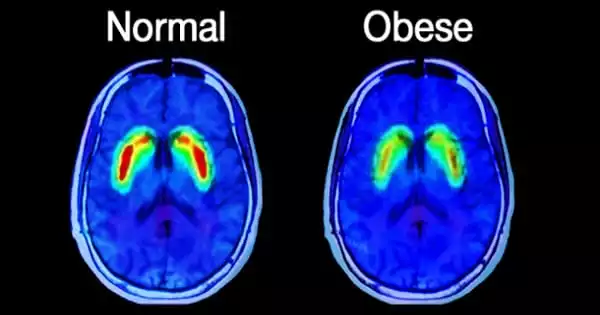
Kantonen’s research looked at changes in the brain during pre-obesity by using PET imaging to look at insulin, opioid, and cannabinoid function. The study’s participants included 41 young men with varying levels of obesity risk factors. The findings revealed that family-related risk factors, such as parents’ obesity or diabetes, were linked to altered insulin signaling in the subject’s brain, as well as reduced opioid and cannabinoid system function.
Because of the high rates of obesity and depression, as well as their individual links to cardiovascular disease, many researchers have begun to investigate the relationship between weight and mood. An examination of 17 cross-sectional studies revealed that people who were obese were more likely to be depressed than those who were healthy weights. Because the studies included in the analysis only assessed weight and mood at a single point in time, the researchers were unable to determine whether obesity increases the risk of depression or depression increases the risk of obesity.
New evidence suggests that the link between obesity and depression is a two-way street: A meta-analysis of 15 long-term studies that followed 58,000 people for up to 28 years discovered that people who were obese at the start of the study had a 55% higher risk of developing depression by the end of the study, and people who had depression at the start of the study had a 58% higher risk of becoming obese.
“Disturbance in the neural networks controlling satiation and appetite can thus be seen before a person develops obesity, and these brain changes are linked to family-related obesity risk factors. The findings may have implications for the development of obesity prevention and treatment interventions. They demonstrate that the brain and central nervous system are important targets for obesity treatment “Kantonen adds.
Obesity, in particular, impairs almost every aspect of health, from reproductive and respiratory function to memory and mood. Obesity raises the risk of a number of debilitating and fatal diseases, including diabetes, heart disease, and some cancers. It accomplishes this via a variety of mechanisms, some as simple as the mechanical stress of carrying extra pounds and others involving complex changes in hormones and metabolism. Obesity reduces life quality and length, while increasing individual, national, and global healthcare costs.
Obesity has a negative impact on almost every aspect of health, from reducing life expectancy and contributing to chronic conditions like diabetes and cardiovascular disease to interfering with sexual function, breathing, mood, and social interactions. Obesity is not always a permanent condition. Weight loss can be achieved through diet, exercise, medications, and even surgery. However, losing weight is far more difficult than gaining it. Obesity prevention, beginning at a young age and continuing throughout one’s life, has the potential to vastly improve individual and public health, reduce suffering, and save billions of dollars in health-care costs each year.