According to the findings of a big study published today (May 31, 2016) in The BMJ, women with migraines have a little higher chance of acquiring cardiovascular disorders, such as heart attacks and strokes, and are slightly more likely to die from these ailments than women without migraines.
According to specialists, these findings add to the notion that migraine should be regarded a significant risk factor for cardiovascular disease. However, additional research is needed to establish plausible causes and whether migraine prevention medicines can assist to lower these chances.
Although migraine has been related to an increased risk of stroke, few studies have found a relationship between migraine and cardiovascular disease or mortality. It’s a headache that usually affects one side of the head and causes extreme throbbing pain or a pulsing sensation.
It’s commonly accompanied by nausea, vomiting, and excessive light and sound sensitivity. As a result, a group of researchers from the United States and Germany conducted a major prospective study to assess the links between migraine, cardiovascular disease, and death.
They looked at information from 115,541 women who took part in the Nurses’ Health Study II. The patients were 25 to 42 years old, free of angina and cardiovascular illness, and were tracked for cardiovascular events, diseases, and mortality from 1989 to 2011.
Migraine is a frequent health problem that affects one out of every five women and one out of every fifteen males. They usually start while a person is in their early twenties. Some migraines can be prevented and made less unpleasant with the use of medication. The correct medications, in combination with self-help treatments and lifestyle adjustments, may be beneficial.
The magnitude of the risk should not be over-emphasized, because it is small at the level of the individual patient, but still important at the population level because migraine is so prevalent.
Rebecca Burch
At the start of the study, 17,531 (15.2%) of the women said they had been diagnosed with migraine by a doctor. Over the course of the study’s 20-year follow-up, 1,329 total cardiovascular disease events occurred, with 223 women dying as a result of the disease.
These findings reveal that women who reported a migraine had a higher risk of serious cardiovascular diseases, such as heart attacks, strokes, and angina/coronary revascularization procedures, as compared to women who did not report a migraine.
After controlling for other factors that could have elevated the risk of these diseases, the relationships remained.
Furthermore, migraine was linked to an increased risk of cardiovascular death. This link was found in all subgroups of women, regardless of their age, smoking status, hypertension, postmenopausal hormone therapy, or use of oral contraceptives.
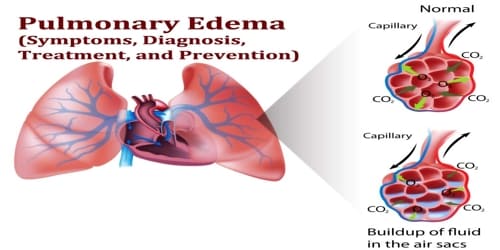
The term “cardiovascular disease” (CVD) refers to any ailment that affects the heart or blood vessels. It’s frequently linked to fatty deposits in the arteries (atherosclerosis) and an elevated risk of blood clots. It’s critical to recognize the cardiovascular illness as soon as possible so that treatment may begin with counseling and medications.
Rebecca Burch of Harvard Medical School and Melissa Rayhill of The State University of New York at Buffalo writes in a companion editorial that “the magnitude of the risk should not be over-emphasized,” because “it is small at the level of the individual patient, but still important at the population level because migraine is so prevalent.”
While the current study took into account a significant number of vascular risk variables, no data on vascular biomarkers or migraine characteristics such migraine aura was provided.
Nevertheless, the authors say “these results further add to the evidence that migraine should be considered an important risk marker for cardiovascular disease, at least in women,” and there is no reason why the findings can’t be applicable to men.
“Given the significant prevalence of migraine in the general population, there is a pressing need to better understand the biological processes at work and to assist patients with preventative options,” they conclude.
The editorialists Rebecca Burch and Melissa Rayhill agree “it’s time to add migraine to the list of early life medical conditions that are markers for later life cardiovascular risk.”
They continue by adding that this latest study raises issues about whether medications that lower the frequency or intensity of migraines can minimize vascular risks later in life, “what little evidence we do have suggests the need for therapeutic restraint to prevent cardiovascular risk until we have a better understanding of the mechanisms underlying the link between migraine and vascular disease.”