Anxiety and depression are both common mental health conditions that can have a significant impact on an individual’s daily life. Anxiety is characterized by feelings of worry, nervousness, or fear that are often out of proportion to the situation at hand. Depression, on the other hand, is characterized by feelings of sadness, hopelessness, and loss of interest in activities.
If you Google “How do antidepressants work” or “Why antidepressants treat anxiety,” the search engine will direct you to a plethora of websites, some of which cater to regular people looking for medical information, others to doctors and academics, but all of which provide answers along the lines of this: “Although we don’t fully understand how this class of drugs works, they likely affect mood by increasing the amount of the neurotransmitter serotonin in mood centers of the brain.”
As a brain scientist, I cringe when reading such explanations, wishing they had stopped at “We don’t fully understand how this class of drugs works.”
The brain does not neatly divide itself into simple constructs such as “mood centers” and “serotonin pathways,” due to its numerous nuclei, interconnected pathways, metabolic processes, immune responses, negative feedback and feed-forward loops, neurogenesis processes, and neurotransmitters, not to mention the psychotropic effects of gut bacteria.
Serotonin
Simply put, we are trying to arrange the brain using these artificial frameworks in order to start understanding it. When we categorize medications like Prozac and Zoloft as selective serotonin reuptake inhibitors (SSRIs), we are equally guilty of oversimplification because these chemicals also cause several other types of changes in the body that may be just as essential as or even more so for lowering symptoms.
For example, although the major class of antidepressants, SSRIs, do slow down synaptic re-uptake of serotonin, at least temporarily increasing serotonin levels, recent studies show there is very little correlation between brain serotonin levels and severity of depressive symptoms.
And, yet, there is abundant evidence that “SSRIs” do alleviate both depression and anxiety in some patients.
So, if serotonin isn’t the whole answer or even part of the answer what is?
The Inflammation Hypothesis
In studies unrelated to psychiatry, depression was first connected to inflammation in the body and brain more than ten years ago. For instance, a large percentage of test subjects in clinical trials of a hepatitis C medication that boosted pro-inflammatory cytokines appeared to develop depression.
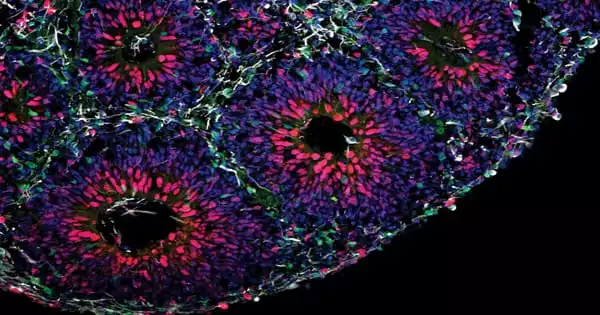
Since those early investigations, a deluge of evidence has linked inflammation to both sadness and anxiety, with researchers thinking that persistent inflammation may be harmful to neurons involved in mood, causing their impairment or possibly eventual destruction. Whatever the mode of action, there is a growing body of studies showing a clear connection between inflammation and both sadness and anxiety.
- Anti-inflammatory drugs can help anxiety and depression: Medications such as aspirin and ibuprofen alleviate depression and anxiety in some patients.
- Exercises like aerobics and meditation that lower anxiety and depression also lower inflammation.
- Antidepressants and anti-anxiety drugs have anti-inflammatory properties: Both SSRIs and antianxiety drugs such as benzodiazepines (e.g., Librium, Valium, Ativan) reduce inflammation. Even psychedelics, such as ketamine and psilocybin, which have shown promising antidepressant/antianxiety properties, have anti-inflammatory features.
- Drugs that promote inflammation can worsen depression and anxiety: Immunotherapies that target cancer and viruses are associated with elevated levels of anxiety and depression in certain patients.
- Inflammatory disorders correlate with depression and anxiety: Anxiety and depression symptoms are worse than usual in people with autoimmune disorders include allergies, asthma, multiple sclerosis (MS), rheumatoid arthritis, and diabetes.
Together, these results provide clear evidence that drugs and behaviors that produce inflammation raise the risk of anxiety and depression, whereas conversely, agents and behaviors that lower inflammation also lower the risk of both conditions.
The findings also raise intriguing questions:
- Considering that viruses may be responsible for causing other brain illnesses like MS, schizophrenia, and obsessive-compulsive disorder, what part do infections play in the onset of depression and anxiety?
- Can diet with inflammatory and anti-inflammatory foods influence mood disorders?
- Can common medications such as aspirin and ibuprofen be prescribed to treat mood disorders?
- Does the role of inflammation in mood disorders help explain why antidepressants don’t help everyone?
- Can antidepressants and anti-anxiety medications be used to treat chronic inflammation?
All of these possibilities should be explored.
The inflammation hypothesis, which is about to replace the serotonin hypothesis, will likely also be replaced by later findings as researchers learn that inflammation doesn’t explain everything, just as the serotonin hypothesis itself replaced an early “catecholamine” (noradrenaline, adrenaline, and dopamine) hypothesis of mood disorders.
I (Eric Haseltine Ph.D.) suspect it will take a long, long time to get the whole story. Our brains are amazing at many things, but one of them is not being able to figure things out for themselves.