There is some evidence to suggest that cholesterol-lowering drugs, also known as statins, may be associated with a lower risk of bleeding stroke. Bleeding stroke, also known as hemorrhagic stroke, is a type of stroke that occurs when a blood vessel in the brain ruptures or leaks. This can cause bleeding in the brain, which can be life-threatening.
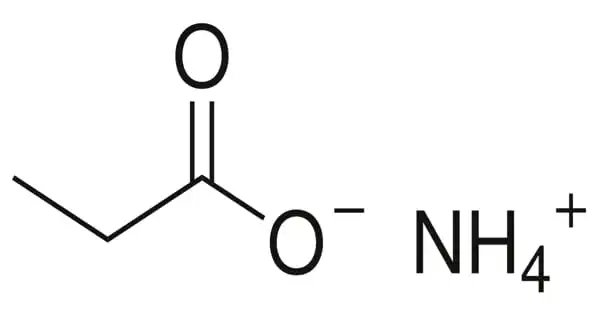
Statins are a type of medication that is commonly used to lower cholesterol levels in the blood. High cholesterol is a risk factor for stroke, so it is thought that statins may help to reduce the risk of stroke by lowering cholesterol levels. Some studies have found that statins may be associated with a lower risk of bleeding stroke, although the evidence is not yet definitive.
It is important to note that the use of statins has been associated with some side effects, including muscle pain and an increased risk of muscle injury. It is important to discuss the potential benefits and risks of taking statins with a healthcare provider before starting treatment.
People who take cholesterol-lowering drugs called statins may have a lower risk of having a type of stroke called an intracerebral hemorrhage, according to a new study published in the December 7, 2022, online issue of Neurology®, the medical journal of the American Academy of Neurology. An intracerebral hemorrhage is caused by bleeding in the brain.
It’s reassuring news for people taking statins that these medications seem to reduce the risk of bleeding stroke as well as the risk of stroke from blood clots. However, our research was done in only the Danish population, which is primarily people of European ancestry. More research should be conducted in other populations.
David Gaist
“While statins have been shown to reduce the risk of stroke from blood clots, there has been conflicting research on whether statin use increases or decreases the risk of a person having a first intracerebral hemorrhage,” said study author David Gaist, MD, Ph.D., of the University of Southern Denmark in Odense and a member of the American Academy of Neurology. “For our study, we looked at the lobe and non-lobe areas of the brain to see if the location was a factor for statin use and the risk of a first intracerebral hemorrhage. We found that those who used a statin had a lower risk of this type of bleeding stroke in both areas of the brain. The risk was even lower with long-term statin use.”
The lobe area of the brain includes most of the cerebrum, including the frontal, parietal, temporal, and occipital lobes. The non-lobe area primarily includes the basal ganglia, thalamus, cerebellum, and brainstem.
For the study, researchers looked at health records in Denmark and identified 989 people with an average age of 76 who had an intracerebral hemorrhage in the lobe area of the brain. They were compared to 39,500 people who did not have this type of stroke and were similar in age, sex, and other factors.
They also looked at 1,175 people with an average age of 75 who had an intracerebral hemorrhage in the non-lobe parts of the brain. They were compared to 46,755 people who did not have this type of stroke and were similar in age, sex, and other factors.
Researchers used prescription data to determine information on statin use.
Of the total participants, 6.8% who had a stroke had been taking statins for five or more years, compared to 8.6% of those who did not have a stroke.
After adjusting for factors like high blood pressure, diabetes, and alcohol use, researchers found that people currently using statins had a 17% lower risk of having a stroke in the lobe areas of the brain and a 16% lower risk of stroke in the non-lobe areas of the brain.
Longer use of statins was associated with a lower risk of stroke in both areas of the brain. When using statins for more than five years, people had a 33% lower risk of having a stroke in the lobe area of the brain and a 38% lower risk of stroke in the non-lobe area of the brain.
“It’s reassuring news for people taking statins that these medications seem to reduce the risk of bleeding stroke as well as the risk of stroke from blood clots,” Gaist added. “However, our research was done in only the Danish population, which is primarily people of European ancestry. More research should be conducted in other populations.”