Latex Allergy Disorder
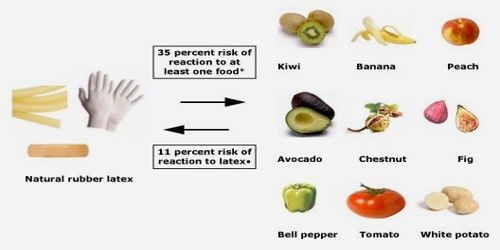
Definition: Latex allergy is defined as the presence of specific immunoglobulin E (IgE) antibody to latex proteins in persons who have a variety of clinical symptoms to latex-containing products. Latex allergy generally develops after repeated exposure to products containing natural rubber latex. As many items contain or are made from natural rubber, including shoe soles, elastic bands, rubber gloves, condoms, baby-bottle nipples, and balloons, there are many possible routes of exposure that may trigger a reaction. People with latex allergies may also have or develop allergic reactions to some fruits, such as bananas.
Latex is a milky sap produced by some plants, including the tropical rubber tree. It is a mixture of water, sugar, and proteins. Plants usually release latex after they are injured, in the same way, that humans bleed following an injury. Plants use latex as a defense against insects. Latex is used in over 40,000 products with many different uses.
Natural latex is usually white but can be scarlet, orange, and yellow. In many modern products, latex is synthesized, rather than being taken from natural sources.
- People who are at higher risk for developing latex allergy include:
- Health care workers and others who frequently wear latex gloves
- People who have had multiple surgeries (for example, 10 or more), such as children with spina bifida
- People who are often exposed to natural rubber latex, including rubber industry workers
- People with other allergies, such as hay fever (allergic rhinitis) or allergy to certain foods
Natural rubber latex is known to cause allergic reactions of Type I (e.g. anaphylaxis) and Type IV (e.g. allergic contact dermatitis) as well as non-allergic irritant contact dermatitis.
Risk Factors: Allergy is defined by sensitization and clinical symptoms. Prevalence rates of latex allergy or sensitization have varied from population to population. The highest rates are found in patients with spina bifida and other congenital urogenital anomalies (24%–60%), moderate rates are found in healthcare workers and employees in the rubber industry (5%–15%), and the lowest rates are found in the general population (1%).4 Irritant dermatitis may be another risk factor for the development of immunologic reactions to latex because the protective skin barrier is altered and allergen exposure and absorption may be increased, leading to possible IgE sensitization.
Causes, Sign, and Symptoms of Latex allergy: Allergic people’s immune systems identify latex as a pathogen – a substance or organism that harms health. The immune system triggers cells in the body to produce antibodies that fight the latex component. The next time the body comes into contact with latex, the antibodies detect it and signal the immune system to release chemicals, including histamine into the bloodstream.

During manufacturing, latex is often modified. Sometimes, the product is not thoroughly washed. As a result, more “free” latex is present on the surface. This “free” latex is responsible for a significant proportion of latex allergies. Free latex easily sticks to the powder that is often used in surgical gloves. During use, the gloves frequently “snap” when putting them on or taking them off. This snapping sends the powder into the air. Inhaled latex can be a serious allergic problem.
Symptoms can range from mild to severe, and can include one or more of the following:
- Hives or welts
- Swelling of the affected area
- Runny nose
- Sneezing
- Headache
- Reddened, itchy or teary eyes
- Sore throat, hoarse voice
- Abdominal cramps
- Chest tightness, wheezing, or shortness of breath (asthma)
If exposure to latex continues, allergy symptoms may include a severe and life-threatening allergic reaction called anaphylaxis.
Diagnosis, Treatment, and Prevention of Latex allergy: A pertinent history for symptoms related to latex exposures, tests to confirm the presence of IgE antibody, are necessary determine latex allergy. Provocative challenges can be completed if needed. The two most common methods used to identify specific IgE antibodies are the percutaneous (prick) skin test and radioallergosorbent test (RAST).

There is no current treatment available to desensitize someone that is allergic to latex. In other words, there is no way to prevent an allergic reaction if somebody is allergic to latex and comes into contact with it.
Allergic reactions are treated with antihistamines, adrenaline, and steroids.
The most effective way to treat this type of allergy is to avoid products containing latex. Patients should learn how to identify and stay away from products that might contain latex. There are other substances that can be used to substitute latex, such as polymers (nitrile, SBR, Butyl, Vitron) and synthetic elastic, such as elastane or neoprene.
If any person has latex allergy they should avoid direct contact with all products and devices that contain latex. Also avoid food that causes an allergic reaction. Latex allergy problems during dental, medical or surgical procedures can be prevented by warning health care providers about latex allergy before any test or treatment. Latex allergic people can receive medical or dental care in a latex-safe area. Hospitals and clinics that use only low protein latex gloves and non-latex gloves have experienced dramatic declines in new cases of latex allergy.
Information Source: