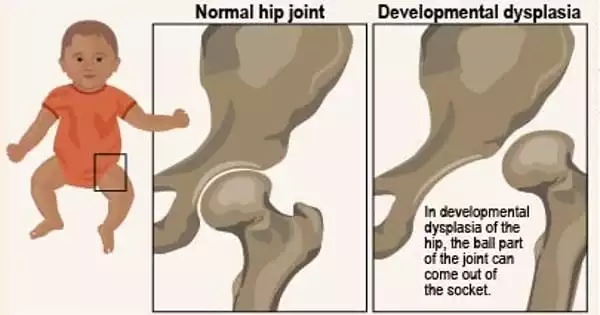
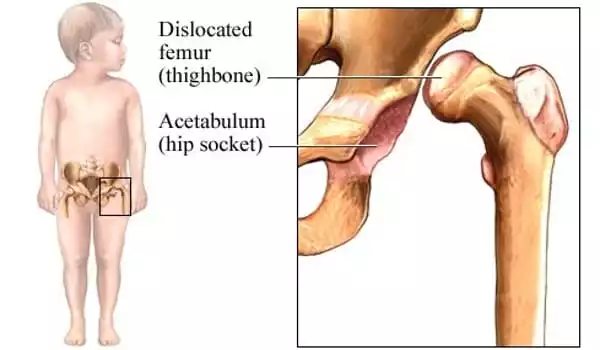
DDH (developmental dysplasia of the hip) is an issue in the formation of a baby’s hip joint. Occasionally the condition develops before the baby is born, and sometimes it develops after the baby is born, as the child grows. It might affect one or both hips. Most DDH infants grow up to be active, healthy children with no hip problems.
According to a study published in Radiology, a technique that uses ultrasound scans to measure the depth and form of the hip socket can effectively predict which infants with hip dysplasia will develop a normal hip structure and which will stay dysplastic. According to the researchers, statistical shape modeling improves existing procedures and may save many infants from unneeded therapy.
Hip developmental dysplasia occurs when the baby’s hip socket is too shallow to cover the thigh bone’s head. In severe situations, the thigh bone might become completely separated from the hip. According to the International Hip Dysplasia Institute, one out of every ten infants is born with hip instability, which means that the hips can be wiggled in the socket due to weak ligaments. The majority of women will naturally tighten up after giving delivery. Hip dysplasia affects one out of every 100 babies.
The financial and logistical challenges for parents and society are the most significant negative outcomes of overtreatment. Medical implications of overtreatment are rather rare, but the danger is not zero; if there is a rare medical consequence, it is most likely avascular necrosis of the hip due to improper treatment device use.
Ralph J. B. Sakkers
There is no agreement on when and how to treat stable hip dysplasia (Graf type 2, as determined by the Graf classification system). Without therapy, it is predicted that approximately 80% of stable Graf 2 hips will evolve to normal. According to study senior author Ralph J. B. Sakkers, M.D., Ph.D., of the Department of Orthopedic Surgery at the University Medical Center Utrecht in Utrecht, the Netherlands, a large percentage of stable cases are likely to be overtreated because there is currently no way to distinguish those who will develop into normal in the future from those who will not. Overtreatment has serious consequences.
“The financial and logistical challenges for parents and society are the most significant negative outcomes of overtreatment,” Dr. Sakkers added. “Medical implications of overtreatment are rather rare, but the danger is not zero; if there is a rare medical consequence, it is most likely avascular necrosis of the hip due to improper treatment device use.”
Avascular necrosis is a condition caused by a temporary or permanent loss of blood supply to the bone. Many kids are born with hips that move freely when they are moved. This is known as neonatal hip laxity. It occurs as a result of the ligaments, which are bands of tissue that connect one bone to another. Neonatal hip laxity normally resolves on its own by the age of 4–6 weeks and is not regarded as real DDH.
Although the Graf classification system is widely used to assess hip dysplasia, it has drawbacks. Patients are divided into groups based on the appearance of the acetabular angle on ultrasound scans. This angle is determined by the depth and form of the hip bone socket into which the femoral head fits. The Graf system is stated to have high variability and low agreement in all reported hip dysplasia parameters, and probe location can impact ultrasound picture quality and anatomic look of the hip.
Statistical shape modeling with ultrasound is an alternate method that quantifies the shape of the image of the hip using several reference points in the 2D ultrasound image, each having an X and Y coordinate. It has the potential to outperform existing predictive models.
“By characterizing the shape of the image of the hip with statistical shape modeling, substantially more data is recovered from the ultrasound images than is currently available,” Dr. Sakkers explained. Dr. Sakkers and colleagues examined the technique’s prediction value in 97 newborns with stable developmental dysplasia of the hip for the study.
They used baseline ultrasound pictures to generate statistical shape modeling, which they then associated with persistent hip dysplasia on ultrasound after 12 weeks of follow-up and residual hip dysplasia on pelvic X-rays around the age of one year.
According to the findings, statistical shape modeling successfully predicted which hips progressed to normal and which remained dysplastic. It also identified hips that benefited from therapy with the Pavlik harness, a soft splint that promotes normal hip socket growth. Although more research is needed to establish the proof of concept, the study findings support statistical shape modeling’s potential involvement in the clinic.
“After confirmation, the procedure may be automated, comparable to the existing automated calculation of skeletal age on X-rays of the hand,” Dr. Sakkers added. The researchers expect that subsequent study in different patient populations with stable hip dysplasia according to the Graf classification will demonstrate the method’s robustness.