A baby is exposed to beneficial bacteria from the mother’s birth canal during a vaginal birth, which helps establish a healthy microbiome. Babies born via C-section, on the other hand, are not exposed to this bacteria and may have a different bacterial colonization pattern.
According to a new study, newborns delivered by cesarean section who are swabbed with their mothers’ vaginal fluid after birth have beneficial bacteria restored to their skin surface and stools. A team of researchers discovered the process, known as vaginal seeding, definitively engrafted new strains of maternal bacteria in the babies’ bodies in the first randomized study of its kind.
According to a new study, newborns delivered by cesarean section who are swabbed with their mothers’ vaginal fluid after birth have beneficial bacteria restored to their skin surface and stools.
A team of researchers led by Rutgers scientists discovered the process, known as vaginal seeding, definitively engrafted new strains of maternal bacteria in the babies’ bodies in the first randomized study of its kind, published in the science journal mBio. These strains would not normally be present in newborns because infants are extracted directly from their mothers’ wombs during C-sections, bypassing the vaginal canal.
Our study is the first double-blind, randomized, placebo-controlled trial to determine whether vaginal seeding causes maternal bacteria to engraft in the skin and stool of neonates.
Maria Gloria Dominguez-Bello
“Our study is the first double-blind, randomized, placebo-controlled trial to determine whether vaginal seeding causes maternal bacteria to engraft in the skin and stool of neonates,” said Maria Gloria Dominguez-Bello, an author of the study and the Henry Rutgers Professor of Microbiome and Health at the Department of Biochemistry and Microbiology in the Rutgers School of Environmental and Biological Sciences (SEBS).
Neonates are infants who are less than 28 days old. In the randomized, blinded study, neither the participants nor the study’s facilitators knew which subjects were receiving the material being studied (in this case, the participating mothers’ vaginal fluids) and who were given a placebo.
“Despite some limitations in this early study, such as a small sample size and only two samples taken over time,” Dominguez-Bello said, “we observed significant effects of vaginal seeding on the neonatal microbiota.”
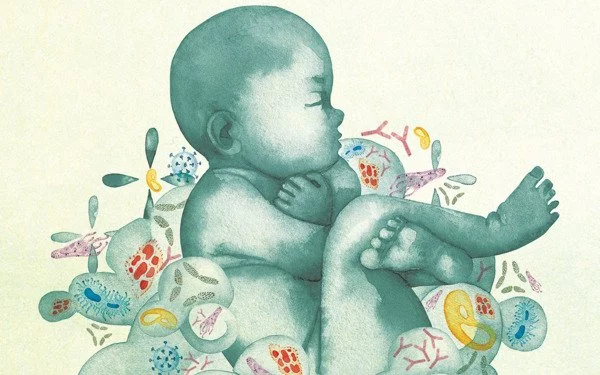
The microbiome is a collection of genomes or essential genetic material from all microorganisms in the environment. The term microbiota typically refers to microorganisms such as bacteria, viruses, and fungi found in a specific environment, such as the skin or the gut. Over the last few decades, scientists have discovered that these collections of microorganisms play an important role in human health, interacting with metabolism, the immune system, and the central nervous system.
Numerous studies have found significant differences in the microbiomes of neonates delivered via C-section versus those born vaginally. According to Dominguez-Bello, some scientists believe that babies born via C-section may miss out on the first live microbes meant to colonize their bodies and sustain their health. A growing body of research shows that preventing microbial colonization during critical early-life developmental windows alters metabolic and immune programming and is linked to an increased risk of immune and metabolic diseases such as asthma, food allergies, obesity, and diabetes.
In the study, the scientists collected microbiota samples from the skin and stool of 20 infants at two different ages: one day old and one month old. They discovered evidence that the maternal microbes had engrafted in the infants. They also discovered that, when compared to the control babies, the babies who received vaginal seeding had a different bacterial population on their skin and in their stool. Their microbiomes contained a pattern of bacterial diversity that was more typical of breastfed babies who were delivered vaginally.
The researchers will continue to assess the babies’ microbiomes for the next five years as part of a larger study, as well as track their growth patterns and whether they develop any markers of metabolic or immune-related disease. The researchers are also expanding the study to include more babies and assess infant health outcomes.