Human Papillomavirus Infection
Definition: Human papillomavirus infection (HPV infection) is an infection by human papillomavirus (HPV) that is passed between people through skin-to-skin contact. Most HPV infections cause no symptoms and resolve spontaneously. In some people, an HPV infection persists and results in warts or precancerous lesions.
Human papillomavirus (HPV) is the most common sexually transmitted infection. Most sexually active men and women being exposed to the virus at some point during their lifetime. There are more than 100 types of HPV that can affect different parts of the body. Some types of HPV can cause warts (such as genital or plantar warts) and others can lead to cancer (such as cervical or anal cancer).
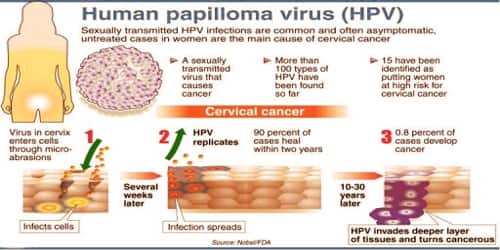
An HPV infection is caused by human papillomavirus, a DNA virus from the papillomavirus family, of which over 170 types are known. More than 40 types are transmitted through sexual contact and infect the anus and genitals. Risk factors for persistent HPV infections include early age of first sexual intercourse, multiple partners, smoking, and poor immune function.
Vaccines can help protect against the strains of genital HPV most likely to cause genital warts or cervical cancer. The majority of HPV infections are generally harmless, though they can be embarrassing. However, the HPV infections that can lead to cervical cancer and other types of cancers are a concern.
Diagnosis and Treatment: There are multiple types of HPV, sometimes called “low-risk” and “high-risk” types. Low-risk types cause warts and high-risk types can cause lesions or cancer. The doctor will make a diagnosis of the skin or genital warts based on a physical exam. Sometimes, the doctor may perform a biopsy (removal of a small tissue sample) to properly diagnose genital warts and eliminate other skin conditions that may be causing the symptoms.

A vinegar solution applied to HPV-infected genital areas turns them white. This may help in identifying difficult-to-see flat lesions.
Theoretically, the HPV DNA and RNA tests could be used to identify HPV infections in cells taken from any part of the body. However, the tests are approved by the FDA for only two indications: for follow-up testing of women who seem to have abnormal Pap test results and for cervical cancer screening in combination with a Pap test among women over age 30.
A vinegar solution applied to HPV-infected genital areas turns them white. This may help in identifying difficult-to-see flat lesions. According to the Centers for Disease Control and Prevention, the body’s immune system clears HPV naturally within two years for 90% of cases. However, experts do not agree on whether the virus is completely eliminated or reduced to undetectable levels, and it is difficult to know when it is contagious.
Medications to eliminate warts are typically applied directly to the lesion and usually take many applications before they’re successful. Examples include:
- Salicylic acid.
- Imiquimod (Aldara, Zyclara).
- Podofilox (Condylox).
- Trichloroacetic acid.
Surgical and other procedures –
If medications don’t work, the doctor might suggest removing warts by one of these methods:
- Freezing with liquid nitrogen (cryotherapy)
- Burning with an electrical current (electrocautery)
- Surgical removal
- Laser surgery
Follow up care is usually recommended and practiced by many health clinics. Follow-up is sometimes not successful because a portion of those treated does not return to be evaluated. In addition to the normal methods of phone calls and mail, text messaging and email can improve the number of people who return for care.

Preventions of HPV infection: It’s difficult to prevent HPV infections that cause common warts. If people have a common wart, they can prevent the spread of the infection and formation of new warts by not picking at a wart and not biting their nails. To reduce the risk of contracting HPV infections that cause plantar warts, wear shoes or sandals in public pools and locker rooms.
Methods of reducing the chances of infection include sexual abstinence, condoms, and vaccination.
The HPV vaccines can prevent the most common types of infection. To be effective they must be used before an infection occurs and are therefore recommended between the ages of nine and thirteen.
Three vaccines are available to prevent infection by some HPV types: Gardasil, Cervarix, and Gardasil 9. The Centers for Disease Control and Prevention (CDC) recommends routine HPV vaccination for girls and boys ages 11 and 12, although it can be given as early as age 9. It’s ideal for girls and boys to receive the vaccine before they have sexual contact and are exposed to HPV. Research has shown that receiving the vaccine at a young age isn’t linked to an earlier start of sexual activity.
The vaccines provide little benefit to women already infected with HPV types 16 and 18. For this reason, the vaccine is recommended primarily for those women not yet having been exposed to HPV during sex. The World Health Organization position paper on HPV vaccination clearly outlines appropriate, cost-effective strategies for using HPV vaccine in public sector programs.
Teens and young adults who begin the vaccine series later, at ages 15 through 26, should continue to receive three doses of the vaccine. Researchers are working on newer vaccines, some designed to treat HPV lesions, but they’re not yet available.
Information Source: