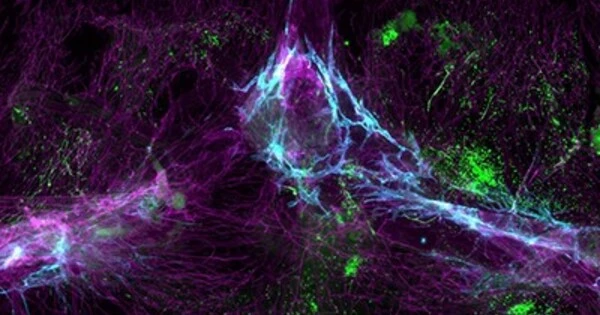
The brain can sense infection through several mechanisms. When the body is infected, immune cells release chemicals called cytokines that activate the brain’s immune cells and trigger a response from the nervous system. The brain also has specialized immune cells called microglia that can detect the presence of pathogens and activate an immune response.
A new study led by Harvard Medical School researchers sheds light on how the brain detects an infection in the body. The researchers discovered that a small group of neurons in the airway plays a critical role in alerting the brain to a flu infection while studying mice. They also discovered evidence of a second pathway from the lungs to the brain that activates later in the infection.
Nature published the findings. Despite the fact that most people get sick several times a year, scientific understanding of how the brain induces sickness has lagged behind research on other bodily states such as hunger and thirst. The paper is an important first step toward understanding the brain-body connection during an infection.
“This study helps us begin to understand a basic mechanism of pathogen detection and how it’s related to the nervous system, which has been largely mysterious until now,” said senior author Stephen Liberles, professor of cell biology at HMS and Howard Hughes Medical Institute investigator.
The findings also shed light on how nonsteroidal anti-inflammatory drugs (NSAIDs) like ibuprofen and aspirin can help with influenza symptoms. If the findings can be applied to humans, the research could have significant implications for developing more effective flu treatments.
This study helps us begin to understand a basic mechanism of pathogen detection and how it’s related to the nervous system, which has been largely mysterious until now.
Stephen Liberles
An infectious state of mind
The Liberles lab is curious about how the brain and body communicate in order to control physiology. It has previously investigated how the brain processes sensory information from internal organs, as well as how sensory cues can elicit or suppress nausea.
The researchers turned their attention in the new paper to another important type of sickness that the brain controls: respiratory infection sickness. During an infection, the brain orchestrates symptoms while the body mounts an immune response, according to Liberles. These can include general symptoms like fever, loss of appetite, and lethargy, as well as more specific symptoms like congestion or coughing for a respiratory illness or vomiting or diarrhea for a gastrointestinal bug.
The team decided to focus on influenza, a respiratory virus that causes millions of illnesses and medical visits each year as well as thousands of deaths in the United States. First author Na-Ryum Bin, an HMS research fellow in the Liberles lab, identified a small population of neurons embedded in the glossopharyngeal nerve, which runs from the throat to the brain, through a series of mouse experiments.
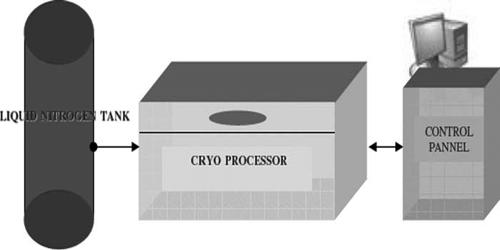
Importantly, he discovered that these neurons, which have receptors for lipids called prostaglandins, are required to signal to the brain that a flu infection is present. During an infection, both mice and humans produce these lipids, which are targeted by drugs such as ibuprofen and aspirin.
Cutting the glossopharyngeal nerve, removing the neurons, blocking the prostaglandin receptors in those neurons, or administering ibuprofen to the mice all reduced influenza symptoms and increased survival. The findings suggest that these airway neurons detect prostaglandins produced during a flu infection and act as a communication link between the upper part of the throat and the brain.
“We believe that these neurons relay information about the presence of a pathogen and initiate neural circuits that control the sickness response,” Liberles explained.
The findings explain how drugs like ibuprofen and aspirin work to reduce flu symptoms, and they suggest that these drugs may even improve survival. The researchers discovered evidence of yet another possible sickness pathway, this time from the lungs to the brain. It appears to become active in the second phase of infection as the virus infiltrates deeper into the respiratory system, according to the researchers.
The team was surprised to discover that this additional pathway does not involve prostaglandins. Ibuprofen had no effect on mice in the second stage of infection. The findings suggest an opportunity for better flu treatment if scientists can develop drugs that target the additional pathway, according to the authors.
A foundation for future research
Liberles and colleagues are eager to investigate a number of questions raised by the study. The first is how well the findings will be applicable to humans. Although mice and humans share a lot of basic sensory biology, including a glossopharyngeal nerve, Liberles stressed that more genetic and other experiments are needed to confirm that humans have the same neuron populations and pathways as mice.
If the findings are replicated in humans, it opens the door to developing flu treatments that target both the prostaglandin- and non-prostaglandin pathways. “It would be incredibly exciting and potentially transformative if you could find a way to inhibit both pathways and use them in synergy,” Liberles said.
Bin is already delving into the details of the nonprostaglandin pathway, including the neurons involved, in order to figure out how to block it. He also wants to identify and study the airway cells that produce prostaglandins in the initial pathway.
Liberles is eager to investigate the full range of disease pathways in the body to determine whether they specialize in different types and sites of infection. He believes that a better understanding of these pathways can help scientists learn how to manipulate them to treat a variety of illnesses.