Folie à deux
Folie à deux is a rare psychiatric occurrence in which one person’s psychotic symptoms, such as delusions, are transmitted to another person. Literally means “madness shared by two” in French; the disorder is also known as ‘shared psychotic disorder’. It is a mental disorder that two people share and experience at the same time. If you and your best friend are convinced that her dog can speak English, it may be a folie a deux.
Recent psychiatric classifications refer to the syndrome as shared psychotic disorder (DSM-IV – 297.3) and induced delusional disorder (F24) in the ICD-10, although the research literature largely uses the original name. This disorder is not in the current DSM (DSM-5). The disorder was first conceptualized in 19th-century French psychiatry by Charles Lasègue and Jean-Pierre Falret and is also known as Lasègue-Falret syndrome.
This unusual disorder is more likely to occur in a closely related pair, like twins, or a married couple, who are isolated from other people. Folie à deux means “shared madness,” or “madness for two” in French. If three people share the delusion, it’s a “folie a trois.”
People with psychotic disorders have trouble staying in touch with reality and often can’t handle daily life. The most obvious symptoms are hallucinations (seeing or hearing things that aren’t real) and delusions (believing things that aren’t true, even when they get the facts).
Causes, Symptoms and Risk factors – The principal feature of shared psychotic disorder is the unwavering belief by the secondary partner in the dominant partner’s delusion. The delusions experienced by both primary partners in shared psychotic disorder are far less bizarre than those found in schizophrenic patients; they are, therefore, believable.
Shared psychotic disorder is mostly observed among people who live in close proximity and in close relationships. It is found in parent-offspring, sibling-sibling, or husband-wife constellations. Furthermore, a mother-daughter or sister-sister pair represents fifty percent of the psychotic dyads. Rarely all the family members share the same delusions, and this is called Folie à famille. Additionally, there are case reports of physician-patient folie à deux and even a case involving a dog.
Risk factors include female gender, mental retardation, suggestibility, passivity, histrionic personality traits, and suspiciousness, in the secondary patient. Moreover, dependency, ambivalent relationships, and repetitive crises have been seen in the family.
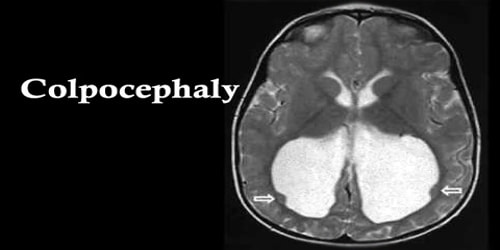
Diagnosis, Treatment, and Prevention – There are no lab tests that specifically diagnose shared psychotic disorders. So doctors may use tools such as brain imaging (including MRI scans) and blood tests to rule out other causes. This syndrome is most commonly diagnosed when the two or more individuals concerned live in proximity and may be socially or physically isolated and have little interaction with other people. Various sub-classifications of folie à deux have been proposed to describe how the delusional belief comes to be held by more than one person :
- Folie imposée is where a dominant person (known as the ‘primary’, ‘inducer’ or ‘principal’) initially forms a delusional belief during a psychotic episode and imposes it on another person or persons (known as the ‘secondary’, ‘acceptor’ or ‘associate’) with the assumption that the second person might not have become deluded if left to his or her own devices. If the parties are admitted to hospital separately, then the delusions in the person with the induced beliefs usually resolve without the need of medication.
- Folie simultanée describes either the situation where two people considered to suffer independently from psychosis influence the content of each other’s delusions so they become identical or strikingly similar or one in which two people “morbidly predisposed” to delusional psychosis mutually trigger symptoms in each other.
The treatment approach most recommended is to separate the secondary partner from the source of the delusion. If symptoms have not dissipated within one to two weeks, antipsychotic medications may be in order.
Once stabilized, psychotherapy should be undertaken with the secondary partner, with an eye toward integrating the dominant partner, once he/she has also received medical treatment and is stable.
In an effort to prevent relapse, family therapy should also be considered to re-establish the nuclear family and to provide social support to modify old family dynamics. The family cannot continue in isolation as it did in the past and will require support from community agencies.
Information Source: