Dyslipidemia
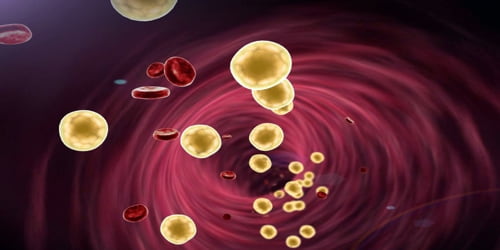
Definition: Dyslipidemia is a medical condition that refers to an abnormal level of blood lipids. In developed countries, most dyslipidemias are hyperlipidemias; that is, an elevation of lipids in the blood. This is often due to diet and lifestyle. Prolonged elevation of insulin levels can also lead to dyslipidemia. Likewise, increased levels of O-GlcNAc transferase (OGT) may cause dyslipidemia.
The most common type of dyslipidemia is hyperlipidemia or high lipid levels. Another, less common form of dyslipidemia, hypolipidemia, refers to lipid levels that are abnormally low. Dyslipidemias can affect any lipid parameter, including LDL cholesterol levels, HDL cholesterol levels, triglycerides, or a combination of these lipids.
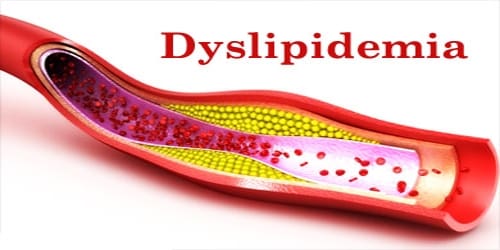
Healthy blood lipid levels naturally vary from person to person. However, people with high levels of LDL and triglycerides or very low HDL levels tend to have a higher risk of developing atherosclerosis.
Atherosclerosis develops when hard, fatty deposits called plaques accumulate in blood vessels, making it difficult for blood to flow.
Over time, these plaques can build up and cause major circulation problems, such as heart attacks and strokes.
Causes and Risk factors of Dyslipidemia: There are many factors that can cause dyslipidemia ranging from inherited disorders to our lifestyle. The causes of dyslipidemia can be divided into two main categories: primary or secondary dyslipidemia.
Primary dyslipidemia: Genetic factors cause primary dyslipidemia, and it is inherited. Common causes of primary dyslipidemia include:
- Familial combined hyperlipidemia, which develops in teenagers and young adults and can lead to high cholesterol.
- Familial hyperapobetalipoproteinemia, a mutation in a group of LDL lipoproteins called apolipoproteins.
- Familial hypertriglyceridemia, which leads to high triglyceride levels.
- Homozygous familial or polygenic hypercholesterolemia, a mutation in LDL receptors.
Secondary dyslipidemia, on the other hand, is more common and occurs due to a variety of factors involving certain aspects of our lifestyle or certain medical conditions people may have. Secondary hyperlipidemias may be caused by:
- Poor or high fat, high sugar diet
- Lack of exercise
- Certain medications such as beta blockers, certain drugs to treat HIV, oral contraceptives
- Liver disease
- Alcohol abuse
- Cigarette smoking
- Hypothyroidism that has not been treated
- Uncontrolled diabetes
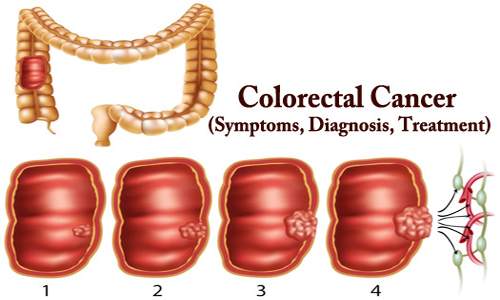
Secondary hypolipidemias, which are less common, may be caused by untreated hyperthyroidism or certain cancers.
Several factors are known to increase the chances of developing dyslipidemia and related conditions. These risk factors include:
- obesity
- a sedentary lifestyle
- a lack of regular physical exercise
- alcohol use
- tobacco use
- use of illegal or illicit drugs
- sexually transmitted infections
- digestive conditions
- older age
- a diet rich in saturated and trans fats
- a parent or grandparent with dyslipidemia
- female sex, as women tend to experience higher LDL levels after menopause
Other medical conditions that can raise your dyslipidemia risk include:
- type 2 diabetes
- hypothyroidism
- chronic kidney or liver conditions
Also, a low HDL cholesterol level is associated with a high LDL level, though the two numbers don’t always move in tandem.
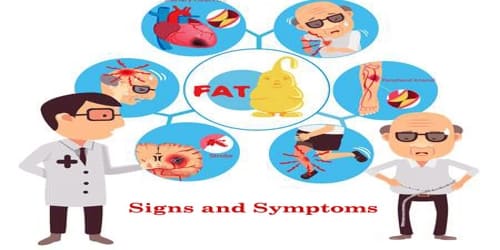
Signs and Symptoms of Dyslipidemia: There is no true way of knowing whether or not people have dyslipidemia whether hyperlipidemia or hypolipidemia unless people have a lipid panel performed. Severe or untreated dyslipidemia can lead to other conditions, including coronary artery disease (CAD) and peripheral artery disease (PAD).
Both CAD and PAD can cause serious health complications, including heart attacks and strokes. Common symptoms of these conditions include:
- leg pain, especially when walking or standing
- chest pain
- tightness or pressure in the chest and shortness of breath
- pain, tightness, and pressure in the neck, jaw, shoulders, and back
- indigestion and heartburn
- sleep problems and daytime exhaustion
- dizziness
- heart palpitations
- cold sweats
- vomiting and nausea
- swelling in the legs, ankles, feet, stomach, and veins of the neck
- fainting
Testing the general population under the age of 40 without symptoms is of unclear benefit. In rare cases of extremely high lipids, raised, yellowish bumps referred to as xanthomas may appear on the body.

Diagnosis and Treatment of Dyslipidemia: A simple blood test that checks for LDL, HDL, and triglycerides will reveal whether people’s levels are high, low, or in a healthy range. These numbers can change from year to year, so getting annual blood work is a good idea. If people take medications for dyslipidemia the doctor may want them to have more frequent blood tests.
There are a variety of treatments and other measures available to address dyslipidemias. Doctors may prescribe one or more lipid-modifying medications for people with very high total cholesterol levels of at least 200 milligrams per deciliter of blood. High cholesterol is usually treated with statins, which interfere with the production of cholesterol in the liver.
If statins fail to lower LDL and triglyceride levels, a doctor may recommend additional medications, including:
- ezetimibe
- niacin
- fibrates
- bile acid sequestrants
- evolocumab and alirocumab
- lomitapide and mipomersen
Some lifestyle changes and supplements can help to encourage healthy blood lipid levels. The first step is to change our diet. Changes should include consuming less saturated fat, refined sugar, and alcohol. Adding more fruits, vegetables, lean proteins, and whole grains to our diet may help. Daily exercise and weight loss may also help us improve our cholesterol profile.
Information Source: