Prostate cancer (PCa) is the leading cause of cancer morbidity and mortality in men worldwide. Despite advances in PCa diagnosis and treatment, a significant proportion of patients with high-risk localized disease, as well as all patients with advanced disease at diagnosis, will develop metastatic castration-resistant prostate cancer (mCRPC).
Critical genomic changes have been identified in response to abiraterone acetate/prednisone, a standard treatment option for men with progressive, incurable, and castration-resistant prostate cancer.
Mayo Clinic researchers identified critical genomic changes in response to abiraterone acetate/prednisone, a standard treatment option for men with progressive, incurable, and castration-resistant prostate cancer, in a new study published in Molecular Cancer Research.
“We defined a potential strategy for both responders and nonresponders of the drug that may help men overcome resistance and prolong survival,” says Liewei Wang, M.D., Ph.D., the Bernard and Edith Waterman Director, Pharmacogenomics Program, Mayo Clinic’s Center for Individualized Medicine. Dr. Wang is the corresponding author of the study.
We defined a potential strategy for both responders and nonresponders of the drug that may help men overcome resistance and prolong survival. Our goal is to integrate these into clinical practice for doctors and patients with castration-resistant prostate cancer.
Liewei Wang
Dr. Wang explains that, while there are several drugs available to control disease progression, many questions remain about which drugs to use in individual cases. Furthermore, predictive biomarkers for drug resistance and sensitivity are largely unknown.
For men with castration-resistant prostate cancer, abiraterone acetate is a standard treatment option. However, the response rate is low, no biomarkers are known to predict prognosis, and alternative therapies for those who fail treatment are not available.
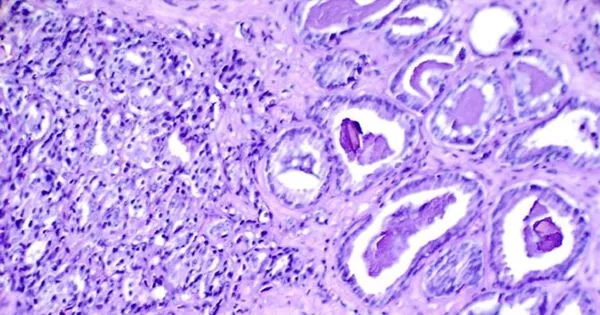
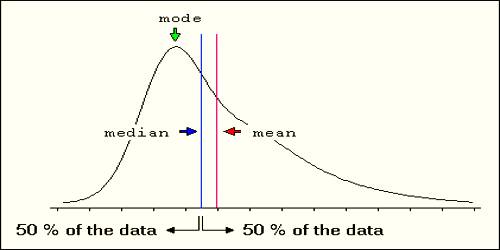
In the Prostate Cancer Medically Optimized Genome Enhanced Therapy study, also known as PROMOTE, Mayo researchers revealed DNA sequences associated with response to abiraterone acetate to identify additional treatment options for men with advanced prostate cancer resistant to all standard therapies. They identified an 11-gene drug panel that provided a new tool to individualize treatment for abiraterone acetate. A genetic testing panel is a laboratory test that looks at a select group of genes. The 11-gene panel predicted a worse prognosis for a subset of primary or metastatic patients enrolled in the study.
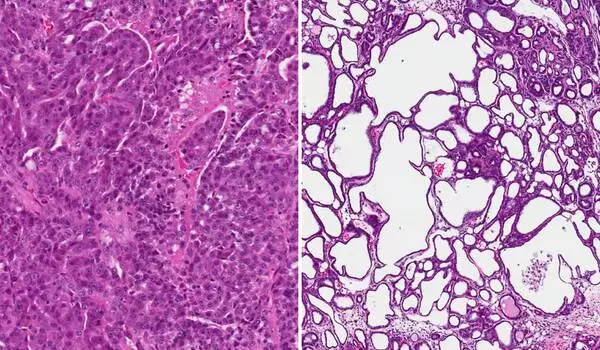
In the next step of their analysis in this prospective study, the researchers analyzed whole-exome sequencing and RNA sequence data from 83 patients with metastatic biopsies before and after 12 weeks of abiraterone acetate/prednisone treatment. They identified genomic alterations associated with acquired resistance after 12 weeks of this treatment.
“We analyzed the posttreatment genomic landscape of metastatic biopsies in these patients with metastatic castration-resistant prostate cancer to identify mechanisms of acquired resistance,” says Hugues Sicotte, Ph.D., a Mayo Clinic bioinformatician and lead author of the study. “These results may assist with selecting alternative therapies in a subset of abiraterone acetate-resistant patients with the highest risk of having the poorest outcome.”
According to Dr. Sicotte, biomarkers based on the stage-specific landscape of genomic changes in prostate cancer are being researched. “Further research will be required to test these drug treatments to overcome abiraterone acetate/prednisone resistance and define nonresponder subgroups,” Dr. Sicotte says. “Our goal is to integrate these into clinical practice for doctors and patients with castration-resistant prostate cancer.”
Prostate cancer is the most common solid organ malignancy in the United States, with over 268,490 new diagnoses each year and an estimated 34,500 deaths. According to the National Cancer Institute’s Surveillance Epidemiology and End Results Program, it is the second leading cause of cancer deaths in men.