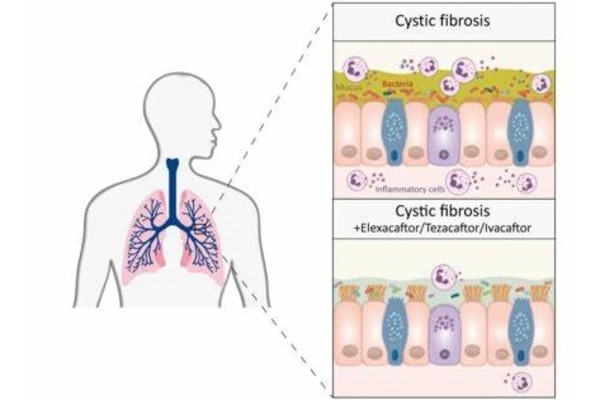
Triple combination therapy is showing encouraging outcomes in improving the health and quality of life of patients with cystic fibrosis (CF). Triple combination therapy normally consists of three drugs: ivacaftor, tezacaftor, and elexacaftor. These medications are intended to target the underlying genetic alterations that cause CF.
Mucus in the airways is less sticky, and inflammation in the lungs is greatly reduced: In patients with cystic fibrosis (CF), triple combination therapy can accomplish these good, long-term outcomes. Researchers from Charité – Universitätsmedizin Berlin and the Max Delbrück Center recently published their findings in the European Respiratory Journal. According to their findings, this type of therapy reduces the symptoms of CF in many people.
Two years ago, a Charité-led study found that a three-drug combination therapy involving elexacaftor, tezacaftor, and ivacaftor is effective in a large proportion of patients with cystic fibrosis, a hereditary disease, meaning that the treatment improves both lung function and quality of life.
Now, a team led by Prof. Marcus Mall, the principal researcher in both studies, has explored for the first time if this type of treatment is also beneficial in the long run, i.e. over a period of 12 months or longer. To investigate this, the researchers examined sputum or secretions from patients’ respiratory tracts.
In patients with cystic fibrosis, the mucus in the airways is very sticky because it doesn’t contain enough water, and the mucins, the molecules that form mucus, adhere too much due to their chemical properties.
Prof. Marcus Mall
“In patients with cystic fibrosis, the mucus in the airways is very sticky because it doesn’t contain enough water, and the mucins, the molecules that form mucus, adhere too much due to their chemical properties. This results in thick, sticky mucus, which clogs the airways, making it harder for patients to breathe and leading to chronic bacterial infection and inflammation of the lungs,” explains Mall, Director of the Department of Pediatric Respiratory Medicine, Immunology and Critical Care Medicine and the Christiane Herzog Cystic Fibrosis Center at Charité.
The current study shows that a combination of elexacaftor, tezacaftor, and ivacaftor leads in less viscous respiratory secretions as well as decreased inflammation and bacterial infection in the lungs of cystic fibrosis patients. “Moreover, the effects lasted for the entire one-year study period. This is critical because previous medications caused a rebound in the bacterial load in the airways,” adds Dr. Simon Gräber, who also works in the Department of Pediatric Respiratory Medicine, Immunology, and Critical Care Medicine at Charité and was one of the study’s co-leaders. The experiment included 79 teenagers and adults with cystic fibrosis and chronic lung disease.
A major step in treating cystic fibrosis, further research important
“This is a major step forward in treating cystic fibrosis,” Mall says. “At the same time, it would be premature to say that patients have been normalized, let alone cured. Chronic lung changes arising over many years of living with the disease cannot be reversed, unfortunately.” This means patients with advanced lung disease will still need to rely on established treatments involving inhaling mucus-thinning medications, taking antibiotics, and physical therapy.
“We plan to forge ahead with our research on how to make treatments that address cystic fibrosis via the molecular defects that cause the disease – like the triple medication combination studied here — even more effective. This includes starting treatment in early childhood with the goal of preventing chronic lung changes wherever possible,” Mall notes.
“Aside from that, this therapy is currently unavailable to about 10% of our patients due to genetic conditions,” Gräber adds. “That is why we are also hard at work on research involving new molecular treatments so that we can effectively treat all people with cystic fibrosis.”
In addition, the researchers are attempting to improve their understanding of mucus problems in cystic fibrosis and to develop new mucolytics, or medications that thin and loosen the mucus. This findings could potentially help patients suffering from prevalent chronic inflammatory lung disorders including asthma and COPD.
Cystic fibrosis
Cystic fibrosis is one of the world’s most common deadly genetic disorders. In Germany now, up to 8,000 children, teenagers, and adults are infected with the disease. People with cystic fibrosis produce thick, sticky secretions that injure organs such as the lungs, gut, and pancreas due to an imbalance in salt and water transport across mucosal surfaces of the body. Despite breakthroughs in treatment, this causes progressive loss of lung function and shortness of breath, which dramatically reduces life expectancy. Every year, 150 to 200 children are born in Germany with this rare condition.