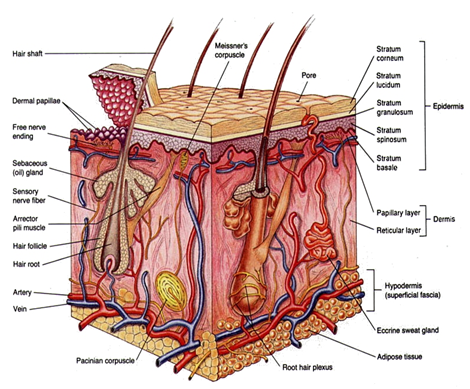
Sulphadiazine fluids by evaporation and loss of excess body heat. Sweat glands help maintain body temperature by controlling the amount of water that evaporates. The dermis is also interlaced with sensory nerve endings that mediate the sensations of touch, pressure, pain, heat, and cold. This is a protective mechanism that allows an individual to adapt to changes in the physical environment. The two layers of the dermis are the papillary and reticular layers. The upper, papillary layer, contains a thin arrangement of collagen fibers. The lower, reticular layer, is thicker and made of thick collagen fibers that are arranged parallel to the surface of the skin. The skin produces vitamin D, which is synthesized by the action of sunlight on certain intradermal cholesterol compounds. Iodine and Silver
Pathology & Pathophysiology of Thermal Injuries
Burn causes coagulative necrosis of the epidermis and underlying tissues, with the depth depending on the temperature to which the skin is exposed and the duration of exposure. The specific heat of the causative agent also affects the depth.
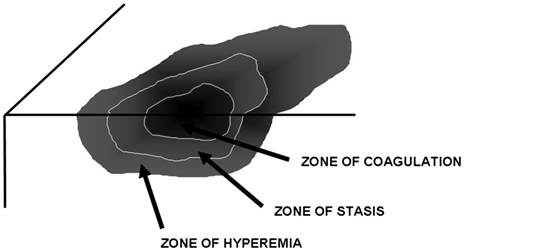
The microscopic pathologic feature of the burn wound is principally surface coagulation necrosis. Jackson’s 1947 state that burned tissue has three distinct zones1.12. The first is the zone of “coagulation,” or necrosis with irreversible cell death and no capillary blood flow. Surrounding this is a zone of injury or stasis, characterized by sluggish capillary blood flow and injured cells. Although damaged, the tissue is still viable. Further tissue
Fig. 3 : Zones of injury. Thermal energy can be visualized as producing three concentric
spheres of injury. The innermost is the zone of coagulation, the middle sphere is
the zone of stasis, and the outermost is the zone of hyperemia.
injury can be caused by products of inflammation such as oxidants and vasconstrictor mediators. Environmental insults such as hypoperfusion, desiccation, or infection can also cause the injured tissue to become necrotic. This process is called wound conversion. The third zone is that of “hyperemia,” which is the usual inflammatory response of healthy tissue to nonlethal injury. Vasodilatation and increased capillary permeability is typically present 8.12.
A rapid loss of intravascular fluid and protein occurs through the heat-injured capillaries. The volume loss is greatest in the first 6–8 hours, with capillary integrity returning toward normal by 36–48 hours. A systemic inflammatory response occurs in response to a large body burn, resulting in the release of oxidants and other inflammatory mediators into unburned tissues. This leads to a shift of extracellular sodium and water into the intracellular space. Smoke inhalation markedly increases the hemodynamic instability, fluid requirements, and mortality rates by adding another source of intense inflammation leading to local lung and systemic tissue damage.
Traditionally, burns have been classified as first-, second-, and third-degree, but the current emphasis on burn healing has led to classification as partial-thickness burns, which can heal spontaneously, and full-thickness burns, which require skin grafting, although deep partial-thickness burns are usually excised and grafted as wel
A first-degree burn involves only the epidermis and is characterized by erythema and minor microscopic changes; tissue damage is minimal, protective functions of the skin are intact, skin edema is minimal, and systemic effects are rare. Pain, the chief symptom, usually resolves in 48–72 hours, and healing takes place uneventfully. In 5–10 days, the damaged epithelium peels off in small scales, leaving no residual scarring. The most common causes of first-degree burns are overexposure to sunlight and brief scalding.
Second-degree or partial-thickness burns are deeper, involving all of the epidermis and some of the corium or dermis. The systemic severity of the burn and the quality of
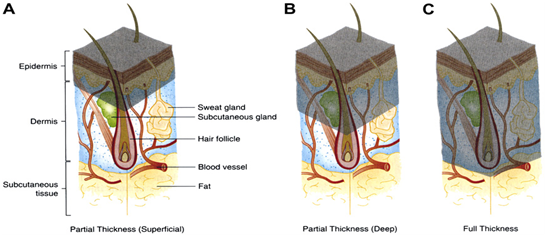
Fig. 4 : Show Classification of burn wounds based on depth of injury.
subsequent healing are directly related to the amount of undamaged dermis. Superficial burns are often characterized by blister formation, while deeper partial-thickness burns have a reddish appearance or a layer of whitish, nonviable dermis firmly adherent to the remaining viable tissue. Complications from superficial second-degree burns are mainly severe pain related. These burns usually heal with minimal scarring in 10–14 days unless they become infected. Deep dermal burns heal over a period of 4–8 weeks .Conversion to a full-thickness burn by bacteria is common. Skin grafting of deep dermal burns, when feasible, improves the biologic quality and appearance of the skin cover.
Full-thickness (third-degree) burns have a characteristic white, dry, waxy appearance and may appear to the untrained eye as unburned skin. Burns caused by prolonged exposure to heat, with involvement of fat and underlying tissue, may be brown, dark red, or black. The diagnostic findings of full-thickness burns are lack of sensation in the burned skin, lack of capillary refill, and a leathery texture that is unlike normal skin. All dermal epithelial elements are destroyed, leaving no potential for reepithelialization.
Topical agents and Burn wound care
Timely and effective use of antimicrobials has revolutionized burn care by decreasing invasive wound infections. An untreated burn wound rapidly becomes colonized with bacteria and fungi because of the loss of normal skin barrier mechanisms. Each wound is dressed with an appropriate covering that serves several functions. First, it protects the damaged epithelium, minimizes bacterial and fungal colonization, and provides splinting action to maintain the desired position of function. Second, the dressing is occlusive to reduce evaporative heat loss and minimize cold stress. Third, the dressing needs to provide comfort over the painful wound .
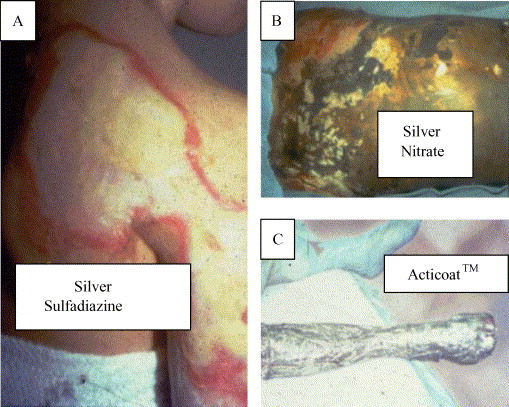
Topical agents have definitely advanced the care of burn patients. Topical antiseptics like silver sulfadiazine, silver nitrate, bacitracin, povidone iodine, chlorhexidine, mupirocine are the most common substances used world -wide in burn care facilities13.14.
Silver sulfadiazine is the most commonly used. It has a broad spectrum of activity because its silver and sulfa moieties cover gram-positive, most gram-negative, and some fungal forms. Some Pseudomonas species possess plasmid-mediated resistance16.17. Silver sulfadiazine is relatively painless on application, has high patient acceptance, and is easy to use. Occasionally, patients complain of a burning sensation after it is applied, and in a few patients, a transient leukopenia develops 3 to 5 days after its continued use. This leukopenia is generally harmless and resolves with or without cessation of treatment18.
PVP-I, which is iodine complexed with polyvinyl pyrolidone19., is a widely used and highly potent antiseptic that eradicates all classes of pathogens responsible for nosocomial infections, including Gram-positive and Gram-negative bacteria, as well as antibiotic-resistant strains and spores (bacterial and fungal), viruses, mycobacteria, and protozoa20. As iodine liberated from the PVP molecule, it exerts its antimicrobial effect in less than a minute, with most organisms being destroyed in 15 to 30 seconds or less21; the mechanisms involved in these effects include an irreversible combination of iodine with tyrosine residues of proteins, interference with the formation of hydrogen bonding by some amino acids and nucleic acids, oxidization of sulphydryl groups, and reaction with sites of unsaturation in lipids 22. All these advantages make PVP-I a good candidate for the topical treatment of burns.
Materials and methods
Study design : A Prospective study.
Place of study : Departments of surgery,
Sher-E-Bangla Medical College Hospital, Barisal.
Study period : August, 2008 to December,2010
Study model : Patients with partial thickness of burn admitted
in the Department of surgery. Sher-E-Bangla
Medical College Hospital, Barisal.
Sample size : 50 cases Partial –thickness of burn caused by
scalding or flames.
Sampling technique: Simple random sampling, lottery method.
Selection criteria:
Inclusion criteria:
These patients with partial-thickness of burn who entered the study had a burn area of 10–40% of total body surface area (TBSA) age > 12yrs caused by scalding or flames.
Exclusion criteria:
Patients who had 3rd degree burns (contact burn and others), contaminated wounds (with chemical or faecal material, or soil), co-morbid diseases, inhalation injury, fractures, neurological injury or who were pregnant and age <12years were excluded from the study. Patient who has reported any allergic reaction to povidone iodine or silver sulfadiazine also excluded from the study.
Study Procedure:
The sample size will be divided in two groups :
Group A(n=25): The first group is the controlled group (i.e. the SSD group) was treated by washing and cleaning with normal saline, followed by topical application of 1% silver sulfadiazine dressing.
Group B(n=25): The second group is the study group (i.e. the PVP-I group) was treated by washing and cleaning with normal saline, followed by topical application of 5% povidone iodine ointment dressing.
The study population included patients of both sexes (male or female) with partial thickness burn admitted to the different units of surgery department of Sher-E-Bangla Medical College Hospital, Barisal from August, 2008 to December, 2010.
Study protocol is approved by the institutional ethical committee of Sher-E- Bangla Medical College, Barisal. The nature of the study was fully explained to each patient and written informed consent was obtained before they were enrollment in the study.
On admission all patients had a full medical history recorded. A complete physical examination was undertaken. The extent, site of the burn and whether superficial or deep was recorded. The cause of the burn was also established. Partial thickness burn defined as superficial partial thickness involved enter epidermis and part of dermis characterized by formation of blister. 50 patients with partial thickness burn were randomized for closed dressing with either 5% PVP-I ointment and 1% SSD cream ( 25 patients in each group). When necessary, analgesics were given and intravenous fluids administered.
During application of the medication to burn wound a record was kept of: (I) the degree of pain experienced (mild, moderate or severe); (ii) the ease of spread of the preparations (excellent, satisfactory or poor); and (iii) the removal of the dressing (easy or difficult).(iv) the number of dressing needed. The respective topical agent was reapplied until the wound had healed. If needed normal saline was used for surgical wash. If antibiotics were required during the study this was recorded. The decision to give antibiotics was based on bacterial culture and sensitivity. Dressing was changed regularly when it was shocked and patient complain discomfort.
Pain recorded according to visual analog pain scale contains a range of numbers starting at 0 and going up to 10. The higher the number, the more intense the pain. On this scale, a 0 indicates that the patient feels no pain. The numbers from 1 to 3 indicate a mild level of pain, numbers from 4 to 7 reflect a moderate degree of pain, numbers from 7 to 10 are reserved for severe pain of an amount that is disabling in nature. The patients compliance about the local antimicrobial agent was recorded during dressing of the burn wound.
The following were checked daily: (i) the patient’s mental state (ii) general condition of the patient, including hydration, temperature; (iii) the degree of wound healing – the wound edge was inspected for evidence of wound infection (secretion of pus) cellulitis, healing was defined as complete epithelialization of the burnt area, and the rate of wound healing was recorded; and (iv) evidence of systemic infection, e.g. septicaemia or abscess formation at distal sites; any other medical complications were also recorded.
Bacterial swabs were taken from the burn surface, 1st at the 5– 7th day then weekly and the cultured organisms identified and antibiotic was advised accordingly.
Patients of both group discharged after complete wound healing and advice for take a follow up after 30 days.
All Data collected by data collection form and they are distributed in a tabulated form for analysis. Quantitative data is analyzed by rate, ratio, proportion and percentage and qualitative data based on works by mean and standard deviation. Significant differences were evaluated using the unpaired Student’s t test and Chi-square test with the help of MS Xcel-07 and SPSS-17. P- Value <0.05 differences were considered as significant level for statistical comparisons.
Ethical measure :
This study protocol was approved by institutional ethical committee of SBMCH, Barisal. All patients were given an explanation of the study and informed consent was taken. The study was not involved any expensive investigative procedures and significant risk, as well as economic burden to the patient.
The study population included patients of both sexes (male or female) of different age group with partial thickness burn admitted to the different units of surgery department of Sher-E-BanglaMedicalCollegeHospital, during the study period.
50 patients with partial thickness burn were randomized for closed dressing with either 5% povidone iodine ointment and 1% silver sulphadiazine ( 25 patients in each group).
The observation is recorded in data collection sheet and distributed in the table for analyze. Quantitative data was analyzed by rate, ratio, proportion and percentage and qualitative data based on works by mean and standard deviation. Significant differences were evaluated using the unpaired Student’s t test and Chi-square test.
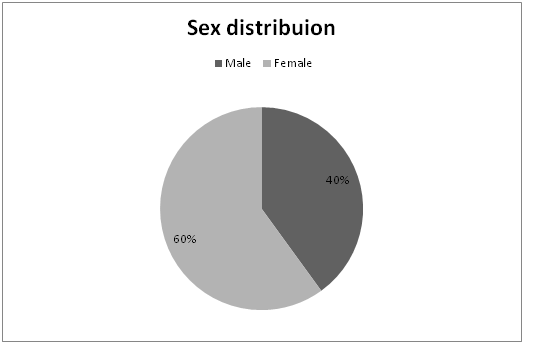
| Table I : Sex distribution of the patients ( n=50 ) | ||||||||
| Sex | Group | Total/percent | ||||||
SSD
Group(n-25 ) PVP-I Group(n=25) Male
9
11
20(40%)
Female
16
14
30(60%)
In this study, SSD group comprises of 9 male and 16 female and in the PVP-I group, 11 male and 14 female patient. This table revels that the incidence of burn was more in female than in the male. Total number of male was 20(40%) and female was 30 (60%).
Fig-5: Show the sex distribution in a pie chart.
In case of burn injury heeling rate is highly depend on early starting of the wound management. In this study the most of the patients ( Group-A, 21 and group-B, 19) came within 6 – 18 hrs, only 3 patients came before 6 hrs and 1 patient came after 24hrs. The mean time of hospital arrival in SSD group is 12.8hrs and PVP-I group 12.6hrs.roup=25 PVP-I
Diagram representing the % TBSA of burn between two study group shown that in case of burn area of 5-20% the number of case was more in SSD Group, but in case of 21-30% burn the number was more in PVP-I group . Most of the patient came with 11-25% burn in both study group. The SSD-group had the highest number of cases in 11-16 % burn, on the other hand the PVP-I group had the highest number in 21-25%.burn.
Table-VII : Distribution of patient compliance during application and removal of the topical antimicrobial agents(n=50)
| ||
During application- Preparations
Spread
SSD Group
n (%)
PVP-I Group
n(%)
Excellent
7(28)
16(64)
Satisfactory
12(48)
7(28)
Poor
6(24)
2(8)
Removal of the preparation
SSD Group
n(%)
PVP-I Group
n(%)
Easy and painless
6(24)
20(80)
Difficult and pain full
19(76)
5(20)
In SSD group among 25 patient, 17(68%) patients complained mild to moderate and 10(40%) patients expressed sever pain experience , in the PVP-I group, 19(76%) patients reported mild to moderate and 6(24%) complained sever pain experience . The mean pain intensity in case of SSD-group was 5.12±0.75 and in the PVP-I group was 4.52±0.77. In chi- quire test the value 2.66 is less than the table value (p=0.05) and is not significant.
Table VII : Represent during application of the topical agent regarding spreading over the burned area the responder compliance for SSD : 7(28% ) excellent, 12(48%) satisfactory and 6(24%) poor, for PVP-I : 16(64%) reported excellent , 7(28%) satisfactorily and 2(8%) poor. The value of chi-squire test ( at df-2 ) 6.838 was more than the table value (p=0.05) difference. So the null hypothesis was rejected. Povidone iodine was well spread during application to the burn wound according to the responder compliance.
During removal of preparation easy and painless reported by 6(24%) cases in SSD group and 20(80%) cases in PVP-I group; Difficult and pain full reported by 19(76%) patient in case of SSD group and 5(20%) patient in PVP-I group.
Count :
Removal of the local agent | Total | ||||
Group of the patient | Easy and painless | Difficult and pain full | Pearson | ||
Chi-Squire test PVP-I
20
5
25
15.705
SSD
6
19
25
Total
26
24
50
proportions compared with the use of Pearson chi-squared test.So the pearson chi-square test value 15.705 , is more than the table value of (p=0.001) with the df-1, so the null hypothesis is rejected and value is highly significant. So PVP-I ointment was more easily and painlessly removable preparation according to responder compliance.
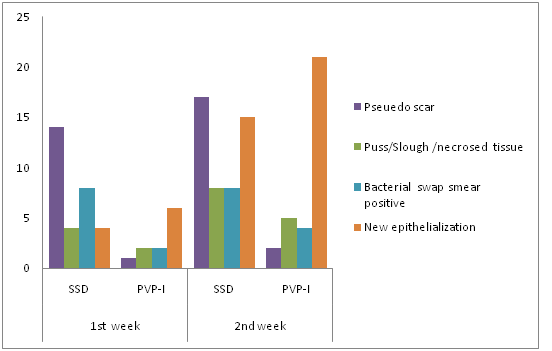
| Table-VIII : Wound observation both group (SSD=25,PVP-I=25) | ||||
Number of cases in 1st week | Number of cases in 2nd week | |||
| Observation | SSD | PVP-I | SSD | PVP-I |
N(%) | N(%) | N(%) | N(%) | |
| Pus/Slough /necrosed tissue | 4(16) | 2(8) | 8(32) | 5(20) |
| Pseuedo scar | 14(28) | 1(4) | 17(68) | 2(8) |
| Bacterial swap smear positive | 8(32) | 2(8) | 8(32) | 4(16) |
| New epithelialization | 4(16) | 6(24) | 15(60 | 21(84) |
The wound of the SSD group shows pus/slough or necrosed tissue in 4 (16%) patient in the 1st week and 8 ( 32%) at the end 2nd week; in the PVP-I group 2 ( 8%) patient at the 1st week and 5 ( 20%) patient at the end of the 2nd week developed the same.
Fig. 8 : Diagram on observation at the end of 1st and 2nd week.
Formation of pseudo scar in 14 ( 56%) at the 1st week and 17 ( 68%) at the 2nd week in patient of SSD group and 1 ( 4%) patient at 1st week and 2 ( 8%) at the 2nd week in PVP-I ; 8 (32%) patients found bacterial smear positive in SSD group and 2 ( 8% ) found in PVP-I at the 1st week; at the 2nd weeks the SSD group found 8 ( 32%) and PVP-I group shown 4 (16%) bacterial positive smear. In SSD group 4 (16%) patient developed new epithelialization within 1st week and 15 (60%) patient at the end of 2nd week, on the other hand in PVP-I group 6 ( 24 %) patient in the 1st week and 21( 84%) at the end of 2nd week developed the same.
| Table IX: Distribution of total number of dressing needed for both group (n=50) | ||
Number of dressing
Number of patient
SSD group (n=25)
PVP-I group (n=25)
10-15
5(20%)
16(64%)
16-20
7(28%)
6(24%)
21-25
13(52%)
3(12%)
Mean dressing number
19.1±2.40
14.9±2.90
Data are given as means ± SD
The table represent the total number dressing of the burn patient were needed during their hospital stay. Maximum number of patients (52%) in SSD group need 21-25 dressing and in the PVP-I group (64%) patient need 10-15 dressing. The mean number of dressing in SSD group 19±2.40 and in the PVP-I group is 14.9±2.90.
| Table X : Distribution of hospital stay of the patients(n=50) | ||
Hospital stay in days Number of patient
SSD group(25)PVP-I group (25)N(%)
N(%)
3- 7days5(20)
6(24)
8-14 days11 (44)
16(64)
15-21days9 (36)
3(12)
MeanHospital stay12.32±3.64
10.40±3.63
Data are given as means ± SD
The most of the patient 16 (64%) in SSD group, 22 (88%) in PVP-I group take discharge in the end of the second week. The mean hospital stay in the SSD group is 12.32±3.64 and in the PVP-I group, the mean hospital stay is 10.40±3.63. In the student’s (unpaired) ‘t’ test value 2.22 is more than the table value of (p=0.05), so null hypothesis is rejected .The Group- B, dressing with PVP-I reduced the significant number of hospital stay.
In the 1st and 2nd week the discharge number is more in Group-B (PVP-I group) and in the 3rd week number was more in Group-A (SSD-group).
All patient advised for follow up after 30 days from the date of discharge only 32 patient response, among them ,18 from the Group-A (SSD Group), 12 patient from the Group-B
( PVP-I group) The table XI show that in the group-A ,among 18 patient,15 case is scar free and 3 case developed scar. In case of group-B among 12 , 11 cases are scar free 1 patient developed scar. Ratio of scar formation among the follow patients in the SSD group is 6: 1; whereas in the PVP-I group 12: 1 The rate of scar formation is two time more in the SSD group of patient among the follow up patient.
It is important to search for locally applicable preparations capable of effectively disinfecting the surface of the burnt area. The principal requirements of such a preparation are that it is non-irritant, painless, easily applied (i.e. spreads well), less expensive, good eschar penetration and is without effect on acid-base balance.Silver sulphadiazine with an excellent spectrum of activity, low toxicity, minimal pain is still the most frequently used topical agent for burn dressing. The use of silver sulphadiazine is frequently associate with the development of pseudo-eschar ,which can lead to error in the evaluation of burn depth by the observer. It does not penetrate eschar, so it is less effective against already established burn wound infections. In this study significant difference between topical use of povidone iodine and silver sulphadiazine was observed during partial thickness burn dressing, the povidone iodine reduces the healing time, the degree of pain experience, rate of eschar formation, the number of dressing , wound infections and duration of hospital stay.
For burn dressing povidone iodine is thus a better option than conventional silver sulphadiazine however, more studies are required to form a conclusion.
Conclusion and recommendation
It is important to search for locally applicable preparations capable of effectively disinfecting the surface of the burnt area. The principal requirements of such a preparation are that it is non-irritant, painless, easily applied (i.e. spreads well), less expensive, good eschar penetration and is without effect on acid-base balance.Silver sulphadiazine with an excellent spectrum of activity, low toxicity, minimal pain is still the most frequently used topical agent for burn dressing. The use of silver sulphadiazine is frequently associate with the development of pseudo-eschar ,which can lead to error in the evaluation of burn depth by the observer. It does not penetrate eschar, so it is less effective against already established burn wound infections. In this study significant difference between topical use of povidone iodine and silver sulphadiazine was observed during partial thickness burn dressing, the povidone iodine reduces the healing time, the degree of pain experience, rate of eschar formation, the number of dressing , wound infections and duration of hospital stay.
For burn dressing povidone iodine is thus a better option than conventional silver sulphadiazine however, more studies are required to form a conclusion.