A recent study has identified a network in the brain associated with resilience to depression. This network involves several brain regions, including the anterior cingulate cortex and the ventromedial prefrontal cortex, and is thought to play a role in regulating emotions and stress responses.
Hope for alternatives to conventional drug-based therapies for mood disorders has been offered by the quickly emerging science of neuromodulation. According to research, these noninvasive techniques can be useful for reducing depressive symptoms and enhancing quality of life. Unfortunately, uncertainty remains about which brain areas to target.
In a new study published October 1, 2022 in the journal Brain, researchers report results from patients with various types of brain injuries that show two distinct brain networks associated with symptoms of depression: one associated with an increase in symptoms (a “risk” network) and one associated with a decrease in symptoms (a “resilience” network).
Brain Networks for Resilience and Risk in Depression
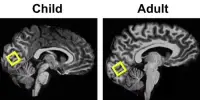
Researchers were able to correlate the locations of brain lesions with levels of depression in the months after the brain injury using brain imaging scans and depression scores from over 500 patients who had sustained localized areas of brain injury (from a stroke or another type of traumatic brain injury).
This lesion mapping method is an effective method for determining the function of different brain areas; if a certain area is damaged and an ability is lost, it is likely that that area is necessary for that ability.
Nodes of the default mode network, which is involved in self-referential thinking or introspection, were shown to be related with regions that experienced less depression. Specifically, peak “resilience” regions included the right medial prefrontal cortex, right orbitofrontal cortex, right inferolateral temporal cortex, and ventral prefrontal white matter tracts.
According to Nicholas Trapp, M.D., University of Iowa Assistant Professor of Psychiatry and lead author of the study, “Previous studies have suggested nodes of this network may be hyperactive in people with depression, who are prone to ruminating. It’s possible that lesions within this network may alter that circuit in a way that leads people to report less depression.”
The salience network, which is involved in emotional processing, attention, and task reorientation, was shown to have nodes in the brain regions that were most strongly associated with greater depression.
Peak “risk” regions included the bilateral dorsolateral prefrontal cortex, left dorsomedial prefrontal cortex, bilateral anterior insula, and dorsal prefrontal white matter tracts.
Average depression scores were found in patients with brain lesions outside of the default mode network or the salience network, who served as the control group. It is believed that this research will result in improved treatments for depression sufferers.
“This could open the doors to potential studies looking at deep brain stimulation, or non-invasive forms of stimulation like TMS, where we might be able to modulate the specific brain areas or networks that we’ve identified, to try to get an antidepressant effect, or potentially other therapeutic effects,” said Trapp.