A new study describes for the first time how a spreading wave of disruption and the flow of fluid in the brain causes headaches, elaborating on the link between the neurological symptoms associated with aura and the migraine that follows. The study also finds novel proteins that may be responsible for headaches and could serve as the basis for new migraine treatments.
“In this study, we describe the interaction between the central and peripheral nervous system brought about by increased concentrations of proteins released in the brain during an episode of spreading depolarization, a phenomenon responsible for the aura associated with migraines,” said Maiken Nedergaard, MD, DMSc, co-director of the University of Rochester Center for Translational Neuromedicine and lead author of the new study, which appears in the journal Science. “These findings provide us with a host of new targets to suppress sensory nerve activation to prevent and treat migraines and strengthen existing therapies.”
It is estimated that one out of every ten persons suffers from migraines, and in around a quarter of these cases, the headache is preceded by an aura, which can involve light flashes, blind spots, double vision, tingling sensations, or limb numbness. These sensations usually develop 5-60 minutes before the headache.
In this study, we describe the interaction between the central and peripheral nervous system brought about by increased concentrations of proteins released in the brain during an episode of spreading depolarization, a phenomenon responsible for the aura associated with migraines.
Maiken Nedergaard
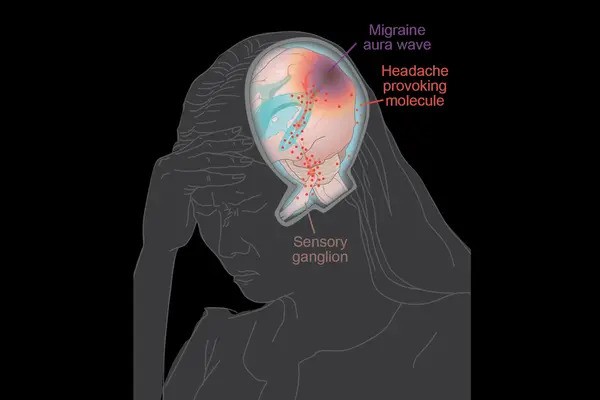
The aura is generated by a phenomenon known as cortical spreading depression, which is a transient depolarization of neurons and other cells induced by glutamate and potassium transport that propagates like a wave across the brain, lowering oxygen levels and hindering blood flow. Most of the time, the depolarization event occurs in the visual processing region of the brain cortex, which causes the visual symptoms that precede a headache.
While migraines auras arise in the brain, the organ itself cannot sense pain. These signals must instead be transmitted from the central nervous system — the brain and spinal cord — to the peripheral nervous system, the communication network that transmits information between brain with the rest of the body and includes sensory nerves responsible for sending information such as touch and pain. The process of communication between the brain and peripheral sensory nerves in migraines has largely remained a mystery.
Fluid Dynamics Models Shed Light on Migraine Pain Origins
Nedergaard and her colleagues at the University of Rochester and the University of Copenhagen are pioneers in understanding the flow of fluids in the brain. In 2012, her lab was the first to describe the glymphatic system, which uses cerebrospinal fluid (CSF) to wash away toxic proteins in the brain. In partnership with experts in fluid dynamics, the team has built detailed models of how the CSF moves in the brain and its role in transporting proteins, neurotransmitters, and other chemicals.
The most widely accepted theory is that nerve endings resting on the outer surface of the membranes that enclose the brain are responsible for the headaches that follow an aura. The new study, which was conducted in mice, describes a different route and identifies proteins, many of which are potential new drug targets, that may be responsible for activating the nerves and causing pain.
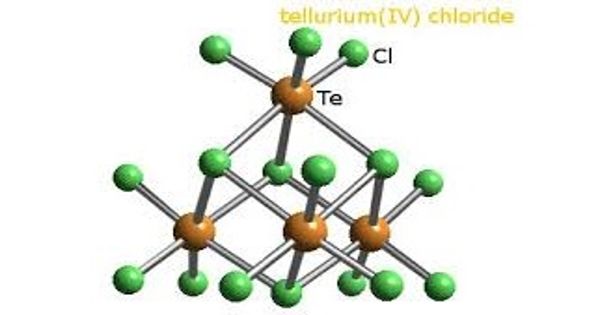
As the depolarization wave spreads, neurons release a variety of inflammatory and other proteins into the CSF. In a series of mouse tests, the researchers demonstrated how CSF carries these proteins to the trigeminal ganglion, a huge bundle of nerves located near the base of the skull that provides sensory input to the head and face.
It was supposed that the trigeminal ganglion, like the rest of the peripheral nervous system, was located outside the blood-brain barrier, which carefully controls what molecules enter and exit the brain. However, the researchers discovered a previously unreported break in the barrier that enabled CSF to flow straight into the trigeminal ganglion, exposing sensory nerves to a cocktail of proteins secreted by the brain.
Migraine-Associated Proteins Double During Brain Wave Activity
The researchers identified twelve proteins known as ligands that bind to receptors on sensory nerves in the trigeminal ganglia, potentially activating these cells. Several of these proteins’ concentrations in CSF more than doubled after a cortical spreading depression. One of the proteins, calcitonin gene-related peptide (CGRP), is already the target of a new class of migraine treatment and prevention medications known as CGRP inhibitors. Other identified proteins are known to play a role in other pain syndromes, such as neuropathic pain, and are most likely involved in migraine headaches as well.
“We discovered a novel signaling route and many chemicals that activate sensory nerves in the peripheral nervous system. Among the identified chemicals are those previously related with migraines, but we didn’t know exactly how and where the migraine-inducing action happened,” said Martin Kaag Rasmussen, PhD, a postdoctoral fellow at the University of Copenhagen and the study’s first author. “Defining the role of these newly identified ligand-receptor pairs may enable the discovery of new pharmacological targets, which could benefit the large portion of patients not responding to available therapies.”
The researchers also observed that the transport of proteins released in one side of the brain reaches mostly the nerves in the trigeminal ganglion on the same side, potentially explaining why pain occurs on one side of the head during most migraines.