According to analyses conducted by a modeling team as part of the Cancer Intervention and Surveillance Modeling Network (CISNET), funded by the National Cancer Institute, if Black women begin mammography screening every other year starting at age 40, breast cancer deaths could be reduced by 57 percent compared to starting screening 10 years later.
Screening mammography is a type of breast imaging that employs low-dose x-rays to detect cancer early, when it is most curable, before women have symptoms. The research is the first to use modeling to determine the best current breast cancer screening procedures for achieving equity in screening outcomes and reducing death disparities.
The study, which was published in Annals of Internal Medicine on October 19, 2021, implies that a reduction in breast cancer fatalities for Black women can be reached with keeping the same benefits-to-harms ratio as when white women begin biennial screening at age 50.
Over the last two decades, recommendations have failed to account for the influence of racism (structural, interpersonal, and internalized) on breast cancer treatment, survival, and deaths among Black women.
“There is an increasing focus on eliminating race-based medicine,” explains the study’s lead author Christina Hunter Chapman, MD, MS, adjunct assistant professor in the Department of Radiation Oncology at the University of Michigan.
“However, calls to end race-based medicine that ask for the immediate cessation of any discussion on race are not likely to eliminate racial disparities. Carefully selected solutions for health inequity may involve tailoring interventions to specific racial groups.”
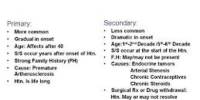
To address this problem, CISNET created a model that uses self-reported race as a proxy for who is likely to be affected by racism in order to test various screening procedures. Breast density, the distribution of breast cancer molecular subtypes, age, stage, and subtype-specific treatment effects, and non-breast cancer mortality for Blacks and whites were all factored into the model.
Black women have higher rates of aggressive cancers at younger ages than white women, and treatments for those types of tumors are not as effective. However, even when we account for cancer subtypes, mortality is higher for black women largely due to factors that are ultimately rooted in racism.
Jeanne S. Mandelblatt
The model compared the benefits and hazards of various screening procedures in Black women to those in white women screened biennially from ages 50 to 74 using all of these data.
“For Black women, three biennial screening strategies (beginning at age 40, 45, or 50) yielded benefit-to-harm ratios that were greater than or equal to those seen in white women who started screening at age 50,” explains Chapman.
“Among those three strategies, initiating mammograms at age 40 yielded the greatest mortality reduction and reduced Black-white mortality disparities by 57 percent. This approach is consistent with the US Preventive Services Task Force’s overarching guidance for when women may want to consider beginning biennial mammography.”
Breast cancer fatalities among women aged 40 to 74 can be reduced with regular screening mammography. This is because they can detect breast cancer early, allowing therapy to begin before it spreads.
The majority of women dislike having a mammogram. Some women find it distressing. Mammography, on the other hand, takes only a few minutes and the discomfort is quickly forgotten.
For women turning 40 in 2020 (i.e., born in the U.S. in 1980), the researchers developed a model to forecast the lifetime impact of digital mammography at various beginning ages and intervals between tests.
It weighed the benefits of early cancer detection (number of years of life gained, breast cancer deaths avoided, and mortality reduction) against the risks of having more mammograms (e.g., annual vs. every other year screening) and false-positive screening results.
Three recent advances in mammography include digital mammography, computer-aided detection, and breast tomosynthesis.
The x-ray film is replaced with electronics that transform x-rays into mammographic photographs of the breast in digital mammography, also known as full-field digital mammography (FFDM). These technologies are comparable to those used in digital cameras, and their efficiency allows for better images while using less radiation.
These breast images are transmitted to a computer for the radiologist’s evaluation and long-term archiving. A digital mammography is identical to a traditional film mammogram in terms of the patient’s experience.
Computer-aided detection (CAD) systems look for anomalous areas of density, mass, or calcification in digitized mammographic pictures that could signal the presence of cancer. The CAD system highlights these spots on the pictures, signaling the radiologist to examine them carefully.
Breast tomosynthesis, also known as three-dimensional (3-D) mammography or digital breast tomosynthesis (DBT), is a type of advanced breast imaging in which several images of the breast are recorded from various angles and reassembled (“synthesized”) into a three-dimensional image set. In this sense, 3-D breast imaging is comparable to computed tomography (CT) imaging, which uses a sequence of thin “slices” to rebuild the body in three dimensions.
Although the radiation dose for some breast tomosynthesis systems is slightly higher than for regular mammography, it is still well within the FDA-approved acceptable levels for mammography radiation. Some systems use dosages that are quite comparable to those used in traditional mammography.
“Black women have higher rates of aggressive cancers at younger ages than white women, and treatments for those types of tumors are not as effective. However, even when we account for cancer subtypes, mortality is higher for black women largely due to factors that are ultimately rooted in racism,” says the study’s senior author, Jeanne S. Mandelblatt, MD, MPH, professor of oncology and medicine at Georgetown Lombardi Comprehensive Cancer Center, and a principal investigator with CISNET.
“Therefore, in our analyses we accounted for differences in treatment attributable to racism, including access to medication, delays in treatment, dose reductions, and discontinuation of treatment all factors that have been shown to be sub-optimal more often in Black than white women,” she adds.
“We hope this provides new information to help develop equity-focused recommendations for Black women and address a long-standing deficit in breast cancer screening guidelines due to the lack of data,” Mandelblatt states.
“In the future, the harms of racism in medicine may be better rectified by developing interventions that use more direct measures of racism as instead of race,” Chapman concludes. “However, using socioeconomic status alone as a proxy for race would not be appropriate in a study like ours given that racial disparities in breast cancer are observed across socioeconomic strata.”
“This project highlights how CISNET modeling can provide important new data to guideline groups seeking to increase equity in cancer outcomes,” says Brandy Heckman-Stoddard, Ph.D., chief, Breast and Gynecologic Cancer Research Group at the National Cancer Institute. “It also points to the need to continue to capture data on screening practices across diverse populations.”