Biliary Colic
Definition
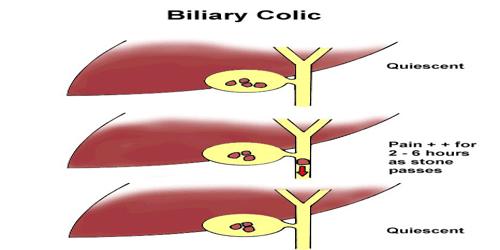
Biliary colic is a type of smooth muscle or visceral pain specifically associated with the passing of stones through the bile ducts, which is also called cholecystalgia. It is also known as a gallbladder attack or gallstone attack. It is caused most frequently by a gallstone becoming impacted in the cystic duct – the tube that is connected to the gallbladder. Biliary colic may also occur due to an impacted stone in the common bile duct (CBD) – the duct that empties bile into the intestine. The pain of biliary colic is often excruciating and may be accompanied by nausea or vomiting. It may last for a few minutes to several hours and may subside spontaneously or with pain relievers.
Bile and digestive enzymes are carried by the bile ducts from the liver, gallbladder, and pancreas to the small intestine. The bile carries away wastes from the liver and helps digest fats. A portion of the bile is stored in the gallbladder. Eating a meal makes the gallbladder contract, or squeeze inward. This empties the gallbladder’s contents into the small intestine.
Treatment for gallbladder attacks (biliary colic) is typically surgery to remove the gallbladder. This can be either done through small incisions or through a single larger incision. Open surgery through a larger incision is associated with more complications than surgery through small incisions. Surgery is typically done under general anesthesia. In those who are unable to have surgery, medication to try to dissolve the stones or shock wave lithotripsy may be tried.
Causes, Sign and Symptoms of Biliary Colic
Biliary colic occurs most frequently due to a gallstone becoming lodged in the cystic duct or CBD. Fluid accumulating behind the obstruction distends the ducts and the gallbladder, which is the main cause of biliary colic. Passage of the stone through the cystic duct or CBD where it may also be the cause of pain. Once the stone moves within the duct so that the obstruction is relieved, or if it passes into the duodenum, the pain is likely to subside.
Cholesterol gallstone formation risk factors include age, female sex, family history, race (e.g. more common in aboriginals), pregnancy, parity, obesity, birth control, diabetes mellitus, cirrhosis, prolonged fasting, rapid weight loss, total parenteral nutrition, ileal disease and impaired gallbladder emptying.
Patients that have gallstones and biliary colic are at increased risk for complications, including cholecystitis. Complications from gallstone disease is 0.3% per year and therefore prophylactic cholecystectomy are rarely indicated unless part of a special population that includes porcelain gallbladder, individuals eligible for organ transplant, diabetics and those with sickle cell anemia.

A person with biliary colic typically feels pain in the middle to right upper abdomen. The pain can feel sharp, crampy, or like a constant dull ache. Colic often occurs in the evening, especially after eating a heavy meal. Some people feel it after bedtime.
Fever and jaundice may occur in case of a stone impacted in the CBD. The pain may subside spontaneously or with analgesics. Biliary colic is likely to recur. Conditions such as gastritis, peptic ulcer, appendicitis, hepatitis, pancreatic disease, angina, and myocardial infarction (heart attack) may be mistaken for biliary colic. Sometimes, one or more of these conditions may occur concurrently, thus making a diagnosis difficult.
The worst pain of biliary colic commonly lasts for 30 minutes to an hour, but may continue at a lower intensity for several more hours. The pain stops when the gallstone breaks free of the bile duct and passes into the intestine.
Diagnosis, Treatment and Preventions of Biliary Colic
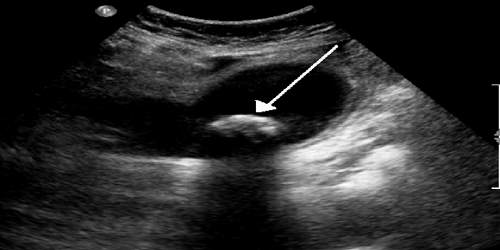
Biliary colic is usually diagnosed from the history and the detection of gallstones. Gallstones are most commonly detected by abdominal ultrasound. Other tests that may also be necessary are:
- Abdominal CT scan.
- Endoscopic retrograde cholangiopancreatography (ERCP) – to locate stones in the CBD.
- Percutaneous transhepatic cholangiogram.
- Endoscopic ultrasound.
- Gallbladder radionuclide scans.
- Magnetic resonance cholangiopancreatography (MRCP).
Blood tests may include bilirubin, liver function tests, and pancreatic enzymes.
The usual treatment for gallstones is surgery to remove the gallbladder. This is known as a cholecystectomy. Laparoscopic surgery, or keyhole surgery, is the most common way to perform a cholecystectomy. It’s often performed as an outpatient procedure. In some cases, open surgery may be required. The surgeon makes an incision in the abdominal area. For this procedure, a hospital stay is required during recovery. Antiemetics, such as dimenhydrinate, are used to treat the nausea. Pain may be treated with anti-inflammatories, NSAIDs such as ketorolac or diclofenac. Opioids, such as morphine, less commonly may be used. NSAIDs are more or less equivalent to opioids. Hyoscine butylbromide, an antispasmodic, is also indicated in biliary colic.
Ursodeoxycholic acid may be useful in preventing gallstones in high-risk patients. Reducing intake of fatty or spicy food may decrease the occurrence of biliary colic.
Reference: