Antibiotic resistance may be exacerbated by microplastics dispersed in the environment. According to one study, chemical-leaching plastics attract bacteria and other vectors, making them susceptible to antibiotic-resistant genes. According to recent Rice University research, microplastic particles may enable bacteria to develop greater resistance to antibiotics. The Styrofoam container that holds your takeout cheeseburger may contribute to the growing resistance to antibiotics in the population.
According to researchers at Rice University’s George R. Brown School of Engineering, discarded polystyrene broken down into microplastics provides a safe haven not only for microbes and chemical contaminants but also for free-floating genetic materials that provide bacteria with resistance.
According to a study published in the Journal of Hazardous Materials, the ultraviolet aging of microplastics in the environment makes them suitable platforms for antibiotic-resistant genes (ARGs). These genes are protected by bacterial chromosomes, phages, and plasmids, all of which can spread antibiotic resistance to humans, reducing their ability to fight infections.
The researcher found that chemicals leaching from the plastic as it ages make vectors more susceptible to horizontal gene transfer, which is how resistance spreads. Microplastic pollution has come to the forefront in recent years as the devastating effects on the environment have become increasingly clear.
Pedro Alvarez
Microplastic pollution has come to the forefront in recent years as the devastating effects on the environment have become increasingly clear. Wastewater treatment plants are a major source of microplastics in the environment, with a typical-sized wastewater treatment plant serving around 400,000 people releasing 2 million microplastic particles into the circulating environment every day. The full extent of the impact of microparticles like these is still unknown, despite the fact that they are found in cosmetics, clothing, food, drinking water, and the air we breathe.
The study, led by Rice civil and environmental engineer Pedro Alvarez in collaboration with researchers from China and the University of Houston, also found that chemicals leaching from the plastic as it ages make vectors more susceptible to horizontal gene transfer, which is how resistance spreads.
“We were surprised to find that microplastic aging improves horizontal ARG,” said Alvarez, the George R. Brown Professor of Civil and Environmental Engineering and director of Rice’s Nanotechnology Enabled Water Treatment Center. “An overlooked potential impact of microplastics pollution is the increased spread of antibiotic resistance.”
The study, published in the Journal of Hazardous Materials, discovered microplastics with diameters ranging from 100 nanometres to five micrometers. Antibiotic resistance is frequently attributed to antibiotic overuse or misuse. However, this new study suggests that resistance can develop even in the absence of antibiotics – bacteria can become more lethal as a result of plastic pollution.
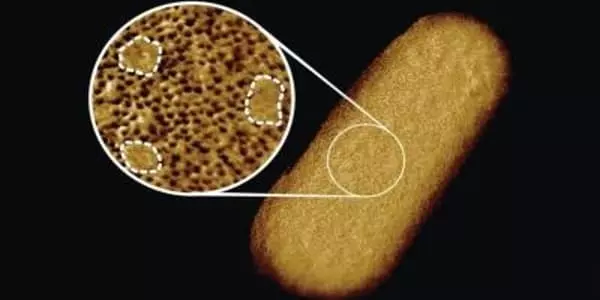
Microplastics (100 nanometers to five micrometers in diameter) aged by the ultraviolet part of sunlight have high surface areas that trap microbes, according to the researchers. As the plastics degrade, they leach depolymerization chemicals into the microbes’ membranes, allowing ARGs to infiltrate.
Plastic particles release chemicals that allow antibiotic-resistance genes (ARGs) to spread as they age. These genes are armed with bacterial chromosomes, phages, and plasmids, which can infect people and cause antibiotic resistance, reducing their ability to fight infections.
“We were surprised to discover that microplastic aging improves horizontal ARG,” says Pedro Alvarez, George R. Brown Professor of Civil and Environmental Engineering and director of Rice’s Nanotechnology Enabled Water Treatment Center.
They discovered that microplastic surfaces can act as aggregation sites for susceptible bacteria, accelerating gene transfer by bringing the bacteria into contact with each other and with chemicals released. According to the study, this synergy could improve environmental conditions favorable to antibiotic resistance even in the absence of antibiotics.
According to the study, microplastics with a surface area of 100 nanometers to 5 micrometers provide an ideal amount of surface area for trapping microorganisms, which are then susceptible to horizontal gene transfer when the plastics degrade and produce depolymerization chemicals. These compounds cause damage to bacteria’s membranes, allowing antibiotic-resistance genes to enter and confer antibiotic resistance on the microbes. The issue is that these microplastics allow bacteria to become more resistant to antibiotics even when antibiotics are not present.
The CDC estimates that more than 2.8 million people in the United States alone are infected with antibiotic-resistant bacteria each year. Antibiotic resistance has frequently been attributed to the overuse or incorrect use of antibiotics as prescribed by medical professionals. According to the most recent research, resistance can develop even in the absence of antibiotics; instead, bacteria can become more resistant to antibiotics and more lethal as a result of pollution.
















