Alzheimer’s disease is characterized by cognitive deterioration, which is often first detected as memory impairment (AD). Deficits in learning, memory, language, and visuospatial skills are caused by neuropathological alterations in the cerebral cortex and limbic system. The distribution of pathogenic alterations in Alzheimer’s disease is reflected in the precise type of cognitive dysfunction. These will fluctuate along the illness severity spectrum and may also be affected by where the disease falls on the dementia spectrum.
Most persons with Alzheimer’s disease have mental health problems in addition to memory impairments and other cognitive symptoms. It has long been debated whether they are the result of brain tissue changes or psychological reactions to cognitive symptoms. A study from Lund University in Sweden has provided new insight, and is published in Biological Psychiatry.
The diagnosis of Alzheimer’s disease is based on cognitive symptoms along with higher levels of specific proteins. At the same time, during the last decade, researchers and physicians have recognized that changes in mood and behavior are frequently extremely early symptoms of the disease. However, these symptoms have received less scientific attention than cognitive problems.
According to our findings, psychiatric symptoms in Alzheimer’s disease could be employed as an alternative outcome measure in therapy studies. This may eventually lead to more successful study design.
Professor Oskar Hansson
Lund University researchers have now looked into the complicated links between psychological symptoms, Alzheimer’s proteins, and cognitive symptoms. This was accomplished as part of Professor Oskar Hansson’s widely recognized BioFINDER investigation.
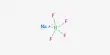
The study included 356 participants over the age of 65 who did not have any cognitive symptoms at the start of the study. Participants’ levels of anxiety, apathy, and overall cognitive function were tested biannually in addition to the levels of the Alzheimer’s proteins amyloid beta and phosphorylated tau in their cerebrospinal fluid. Participants were followed for an eight-year period.
When the data was evaluated, the researchers discovered a definite correlation between high levels of amyloid beta at the start of the study and the development of anxiety and apathy later in life. “Alzheimer’s illness affects large portions of the brain, including the regions that control our emotional life,” explains Maurits Johansson, the study’s principal author.
“Our study shows that psychiatric symptoms, just like cognitive symptoms, occur mainly as a direct consequence of the underlying changes to the brain, due to increased levels of amyloid beta.”

The researchers further demonstrated that amyloid beta drives the development of apathy predominately through direct effects, and that apathy only to a limited extent evolves secondary to cognitive decline. Anxiety was not linked to cognitive change.
“Thus, the findings contradict the notion that early alterations in mood and motivation in Alzheimer’s disease are predominantly psychological responses to cognitive impairment. Instead, the findings show that, at the very least, apathy and anxiety are caused by a pathological accumulation of amyloid beta” Professor Oskar Hansson clarifies
“According to our findings, psychiatric symptoms in Alzheimer’s disease could be employed as an alternative outcome measure in therapy studies. This may eventually lead to more successful study design” He keeps going.
“An earlier BioFINDER study demonstrated that the existence of anxiety or apathy in elderly persons who showed no indications of dementia may indicate an increased risk of future cognitive impairment. As a next step, research is needed to determine how these symptoms may add to the established clinical diagnosis in the early stages of disease, maybe even before cognition is impaired “They reach a conclusion.
The psychological elements of dementia are widely recognized as substantial contributors to discomfort, disability, and care burden and, as a result, are of growing interest to practicing neurologists.
Psychiatric problems, notably depression and schizophrenia, are linked to an increased incidence of dementia in old age. Psychiatric problems, which cause anguish and increase dementia-related deficits, define phenotypes such as frontotemporal dementia and dementia with Lewy bodies. Management necessitates a multidisciplinary team, a problem-solving mindset, care plans, and pharmacologic management. Model programs that give structured problem-solving interventions and individualized in-home care are recent advances.