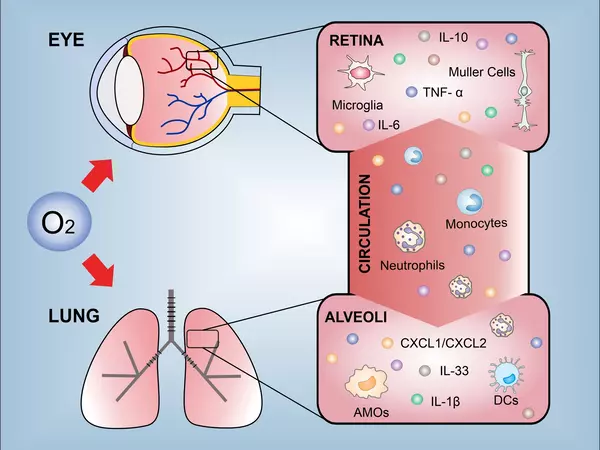
There is increasing evidence to suggest that nerve-immune cell interactions in the lungs play a key role in the development of allergic asthma. Allergic asthma is a type of asthma that is triggered by exposure to allergens, such as pollen or pet dander, which leads to inflammation and narrowing of the airways, making it difficult to breathe.
A new study shows how the interaction of nerves and immune cells in the lungs can contribute to the development of allergic asthma.
Allergic asthma is the most common chronic disease among children, and it can last into adulthood. It is characterized by wheezing and breathing difficulties caused by inhaled allergens such as pollen, mold, and pet dander. Researchers at Massachusetts General Hospital (MGH), a founding member of Mass General Brigham (MGB), have discovered how the relationship between nerves and immune cells in the lungs can contribute to the development of this condition.
Since human lungs are similarly innervated by dopaminergic nerves in early postnatal life, the dopamine-DRD4 axis may provide a therapeutic target to modify allergic asthma progression from childhood to adulthood.
Xingbin Ai
For the study, which is published in the Journal of Allergy & Clinical Immunology, scientists generated unique newborn mouse models of allergen exposure that reproduce the progression of allergic asthma from childhood to adulthood. The worked involved tracking allergen-specific immune cells called T helper 2 resident memory cells (Th2-TRMs) that are known to be the central mediator of recurrent allergic inflammation in the lungs.
Following allergen exposure in newborns, experiments revealed that sympathetic nerves in the lungs produce dopamine and are located near certain T helper 2 cells. Dopamine binds to DRD4 receptors on T helper 2 cells, causing them to be transformed into Th2-TRMs and instructed to produce immune response-stimulating molecules, or cytokines. Blocking this dopamine binding following allergen exposure in newborns reduced the T helper 2 cell transformation and alleviated lung inflammation upon the encounter of the same allergen during adulthood.
“Since human lungs are similarly innervated by dopaminergic nerves in early postnatal life, the dopamine-DRD4 axis may provide a therapeutic target to modify allergic asthma progression from childhood to adulthood,” says senior author Xingbin Ai, PhD, an investigator at MGH and an associate professor of Pediatrics at Harvard Medical School.
“Dopamine signaling is most likely one of several age-related factors that regulate Th2-TRMs in the developing lung. Moving forward, it will be critical to further define the molecular and functional characteristics of pathogenic Th2-TRMs produced in the immature lung. A better understanding of the early life Th2-TRM program’s mediators could lead to the identification of new therapeutic targets for the treatment of allergic asthma.”
Additionally, recent studies have shown that nerve-immune cell interactions can influence the balance of different types of immune cells in the lungs. For example, nerve fibers can stimulate the production of Th2 cells, which are known to play a key role in allergic asthma. Furthermore, nerve-immune cell interactions can also influence the activity of regulatory T cells, which normally help to suppress immune responses and prevent allergic reactions.
Overall, these findings suggest that nerve-immune cell interactions in the lungs are an important factor in the development of allergic asthma. Further research in this area may lead to new treatments that target these interactions and help to alleviate asthma symptoms.