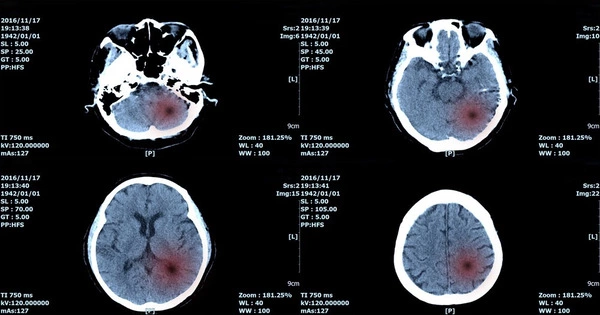
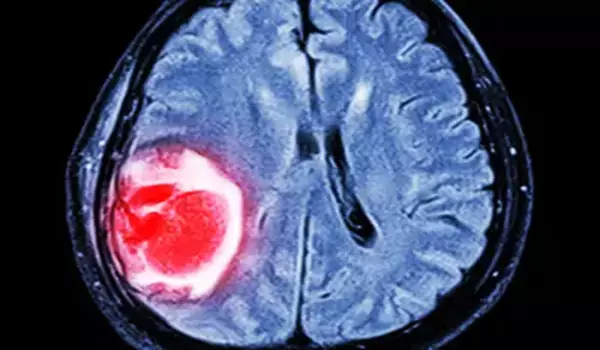
AI is rapidly being used in medical imaging and diagnostics, including the detection and categorization of brain cancers. AI can help healthcare workers make faster and more accurate diagnoses by processing massive amounts of data quickly and efficiently. This has the potential to greatly enhance patient outcomes by allowing for early diagnosis and individualized treatment approaches.
What form of brain tumor is this patient suffering from? AI technologies can assist in determining this as early as 1.5 hours into operation. This procedure usually takes a week. Neurosurgeons can now alter their surgical methods on the fly thanks to new technology. Researchers from UMC Utrecht, as well as pathologists and neurosurgeons from the Princess Máxima Center for Pediatric Oncology and Amsterdam UMC, published their findings in Nature.
In the Netherlands, 1,400 adults and 150 children are diagnosed with a brain or spinal cord tumor per year. Surgery is frequently the initial step in treatment. Neurosurgeons currently do not know what form of brain tumor they are dealing with or how aggressive it is throughout the operation. The exact diagnosis is usually only available one week following surgery after the pathologist has visually and molecularly evaluated the tumor tissue.
Recently, Nanopore sequencing became available: a technology that helps to read DNA in real-time. We created an algorithm capable of learning from millions of simulated realistic ‘DNA snapshots’. We can detect the tumor kind using this technique in 20 to 40 minutes. And that is rapid enough to change the surgical technique directly if necessary.
Jeroen de Ridder
Deep-learning algorithm
UMC Utrecht researchers have created a new ‘deep-learning algorithm,’ a type of artificial intelligence that greatly speeds up diagnosis.
“Recently, Nanopore sequencing became available: a technology that helps to read DNA in real-time,” says Jeroen de Ridder, research group head at UMC Utrecht and Oncode Institute. We created an algorithm capable of learning from millions of simulated realistic ‘DNA snapshots’. We can detect the tumor kind using this technique in 20 to 40 minutes. And that is rapid enough to change the surgical technique directly if necessary.”
Tested and trained with biobank
The Princess Máxima Center’s Pediatric Oncology Laboratory is overseen by Bastiaan Tops. He brought together modern technology and operating room requirements. This was made feasible thanks to support from the KiKa foundation and, more especially, the enormous biobank that the Máxima Center has been maintaining for years. This biobank, among other things, stores tissue from children with brain tumors. The biobank was used to train and test the algorithm.
“The fact that we can now determine the type of brain tumor during surgery demonstrates how technology can speed up diagnostics.” “We’re also looking at how we can use an existing biobank to develop new technology,” Tops explains.
Used during surgery
As a result, the entire technique was repeated numerous times during actual brain surgeries, from taking tissue in the operating room to determining tumor kind. This happened with youngsters in Utrecht and adults in Amsterdam. The operation will take between 60 and 90 minutes in total.
The Princess Máxima Center has determined that the technique’s results are sufficiently dependable and is now utilizing it with children whose surgical strategy may be determined by the outcome. The approach will also be used in regular practice at Amsterdam UMC to help speed up diagnosis.
“During surgery, a small remnant of tumor tissue is sometimes deliberately left behind to prevent neurological damage,” says Eelco Hoving, pediatric neurosurgeon and clinical director of neuro-oncology at the Máxima Center. However, if it is later discovered that the tumor is extremely aggressive, a second surgery may be required to remove the remaining remnant. Patients and their families will face new dangers and stress as a result of this. This can be avoided now because we will already know what type of tumor we are dealing with at the initial surgery.”
Jeroen de Ridder: “It is wonderful that we have been able to actually make the step into clinical practice by combining all areas of expertise, from basic researchers to pathologists and surgeons. By doing so, we can help surgeons to optimize the outcome of brain tumor surgery.”