According to a recent study conducted by experts at Penn State, Stanford University, and an international team of partners, a type of medicine designed for cancer shows promise as a potential treatment for neurological illnesses such as Alzheimer’s.
The researchers discovered that suppressing a specific enzyme known as indoleamine-2,3-dioxygenase 1, or IDO1, allowed them to recover memory and brain function in Alzheimer’s disease models. The findings, published in the journal Science, suggest that IDO1 inhibitors, which are currently being developed as treatments for many types of cancer, including melanoma, leukemia, and breast cancer, could be repurposed to treat the early stages of neurodegenerative diseases, a first for chronic conditions with no preventative treatments.
“We’re showing that there is high potential for IDO1 inhibitors, which are already within the repertoire of drugs being developed for cancer treatments, to target and treat Alzheimer’s,” said Melanie McReynolds, the Dorothy Foehr Huck and J. Lloyd Huck Early Career Chair in Biochemistry and Molecular Biology at Penn State and co-author on the paper. “In the broader context of aging, neurological decline is one of the biggest co-factors of being unable to age healthier. The benefits of understanding and treating metabolic decline in neurological disorders will impact not just those who are diagnosed, but our families, our society, our entire economy.”
Scientists have been targeting the downstream effects of what we identify as an issue with the way the brain powers itself. The therapies that are currently available are working to remove peptides that are likely the result of a bigger issue we can target before those peptides can start forming plaques.
Praveena Prasad
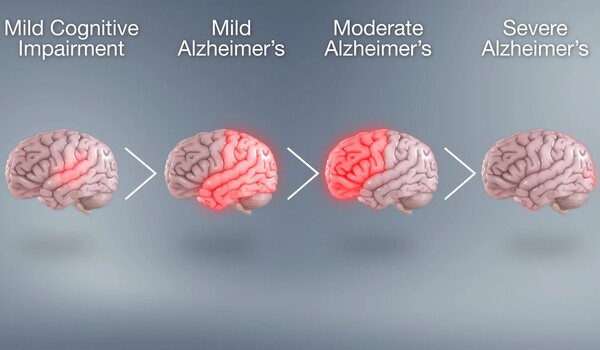
McReynolds noted that Alzheimer’s disease is the most frequent type of dementia, which is a catch-all phrase for all age-related neurodegenerative illnesses. According to the Centers for Disease Control and Prevention, up to 6.7 million Americans had Alzheimer’s disease in 2023, and the frequency is anticipated to quadruple by 2060.
“Inhibiting this enzyme, particularly with compounds that have previously been investigated in human clinical trials for cancer, could be a big step forward in finding ways to protect our brains from the damage caused by aging and neurodegeneration,” said Katrin Andreasson, senior author of the study and the Edward F. and Irene Pimley Professor of Neurology and Neurological Sciences at Stanford University School of Medicine.
Alzheimer’s disease affects the parts of the brain that control thought, memory and language, the result of progressive and irreversible loss of synapses and neural circuitry. As the disease progresses, symptoms can increase from mild memory loss to losing the ability to communicate and respond to the environment. Current treatments for the disease are focused on managing symptoms and slowing progression, through targeting the build-up of amyloid and tau plaques in the brain, but there are no approved treatments for combating the onset of the disease, McReynolds said.
“Scientists have been targeting the downstream effects of what we identify as an issue with the way the brain powers itself,” said Praveena Prasad, doctoral student at Penn State and co-author on the paper. “The therapies that are currently available are working to remove peptides that are likely the result of a bigger issue we can target before those peptides can start forming plaques. We’re demonstrating that by targeting the brain’s metabolism, we can not only slow, but reverse the progression of this disease.”
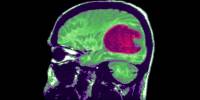
Using preclinical models — in vitro cellular models with amyloid and tau proteins, in vivo mouse models and in vitro human cells from Alzheimer’s patients — the researchers demonstrated that stopping IDO1 helps restore healthy glucose metabolism in astrocytes, the star-shaped brain cells that provide metabolic support to neurons.
IDO1 is an enzyme that converts tryptophan, the sleep-inducing chemical found in turkey, into kynurenine. The body’s creation of kynurenine is the first step in a chain reaction known as the kynurenine pathway, or KP, which is crucial in how the body supplies cellular energy to the brain. The researchers discovered that when IDO1 produced too much kynurenine, it inhibited glucose metabolism in astrocytes, which is essential to power neurons. With IDO1 reduced, metabolic support for neurons improved, restoring their function.
The researchers conducted the investigation in many Alzheimer’s disease models, including amyloid or tau buildup, and discovered that inhibiting IDO1 had protective benefits across both pathologies. Their findings suggest that IDO1 may also be relevant in diseases with other types of pathology, such as Parkinson’s disease dementia and the broad spectrum of progressive neurodegenerative disorders known as tauopathies, according to Paras Minhas, a current resident at Memorial Sloan Kettering Cancer Center who earned a combined medical and doctoral degree in neuroscience at Stanford School of Medicine and is the paper’s first author.
“The brain is very dependent on glucose to fuel many processes, so losing the ability to effectively use glucose for metabolism and energy production can trigger metabolic decline and, in particular, cognitive decline,” Minhas said. “Through this collaboration we were able to visualize precisely how the brain’s metabolism is impacted with neurodegeneration.”