In a struggle that is likely familiar to dieters worldwide, the less a Caenorhabditis elegans (C. elegans) worm consumes, the slower it burns fat. Scripps researchers have now identified why: while fasting, a tiny chemical produced by the worms’ intestines goes to the brain and blocks a fat-burning signal.
Although the specific molecule they discovered in the worms has yet to be examined in humans, the new findings help scientists better comprehend the complicated interaction between the stomach and the brain. It may also shed light on why fasting (not eating for specific periods of time) produces benefits that are unrelated to the number of calories consumed. The latest study appeared in Nature Communications.
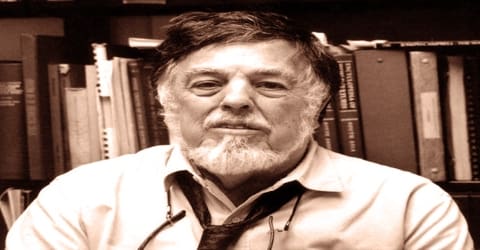
“We’ve found for the first time that fasting is conveying information to the brain beyond just caloric withdrawal,” says Scripps Research Professor of Neuroscience Supriya Srinivasan, PhD, the senior author of the new study. “These findings make me wonder whether there are molecules made in the guts of other animals, including mammals, that explain some of the health outcomes associated with fasting.”
We’ve found for the first time that fasting is conveying information to the brain beyond just caloric withdrawal. These findings make me wonder whether there are molecules made in the guts of other animals, including mammals, that explain some of the health outcomes associated with fasting.
Supriya Srinivasan
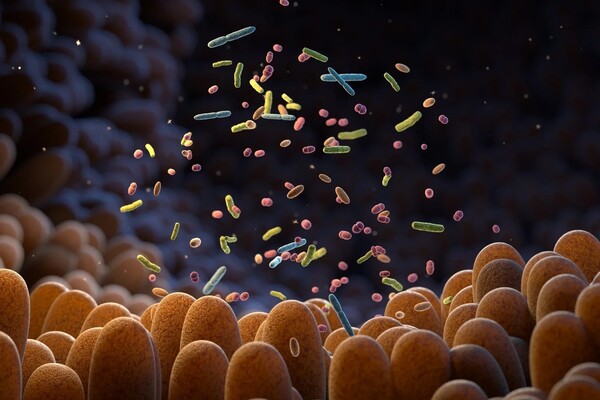
Researchers have long known that the brain regulates fat formation and breakdown in humans, other mammals, and model organisms like C. elegans. In 2017, Srinivasan’s lab discovered FLP-7, a brain hormone that causes fat burning in the roundworm gut. However, because C. elegans’ intestines lack sensory nerves, scientists have failed to identify the reverse communication pathway: how does the stomach inform the brain?
“We knew that altering the metabolic state of the gut could change the properties of neurons in the brain, but it was very mysterious how this actually happened,” according to Srinivasan.
In the new work, Srinivasan and her colleagues removed more than 100 signaling molecules from C. elegans intestines, one at a time, and measured their impact on the brain’s production of FLP-7. They found one molecule that had a large effect on FLP-7: a form of insulin known as INS-7. In humans, insulin is most known as the hormone produced by the pancreas that control blood sugar levels. But this insulin molecule was instead being made by gut cells and also impacting fat metabolism via the brain.
“When we first found that this was an insulin, we thought it was paradoxical,” recalls Srinivasan. “Insulin is so well studied in mammals, and there was no precedent for an insulin molecule having this role.”
However, when the scientists investigated how INS-7 affected FLP-7-producing brain cells, they discovered that it did not activate insulin receptors, as all previously identified insulin molecules do, but rather blocked them. As a result, this barrier triggered a series of subsequent biochemical events that finally caused brain cells to stop generating FLP-7.
“INS-7 is basically a signal coming from the intestines that tells the brain not to burn any more fat stores right now because there’s no food coming in,” Srinivasan says.
Previous research has revealed that fasting can have a number of effects on the body, but the mechanisms underlying these effects are unknown. The new study points toward one way that an empty gut can signal the brain, which could potentially lead to a variety of health impacts beyond fat.
According to Srinivasan, the new findings contribute to understanding how the brain and digestive system communicate in both directions to govern metabolism based on food availability. More research is needed to determine the particular pathways involved in novel gut-to-brain communication in mammals. Compounds that imitate gut hormones, such as semaglutide, also known by the brand names Ozempic, Wegovy, and Rybelus, have lately emerged as popular methods of controlling obesity and diabetes, thus new gut peptides may join this therapeutic class. Srinivasan is also planning tests to investigate how C. elegans gut cells are induced to create INS-7 during fasting and whether types of brain cells are affected by the chemical.