In order to significantly improve the effectiveness of the medication given to women with the potentially fatal condition known as ectopic pregnancy, which happens when a fertilized egg implants somewhere other than the lining of the uterus, researchers at Oregon State University College of Pharmacy have developed a drug delivery system.
Olena Taratula of the Oregon State University College of Pharmacy, and Maureen Baldwin and Leslie Myatt of Oregon Health & Science University led a team that used a mouse model to show that the drug, methotrexate, ends pregnancy at a comparatively low dose when administered via nanoparticles known as polymersomes. Findings were published in the journal Small.
Ectopic pregnancy is the main cause of maternal death in the first trimester and is not viable. Methotrexate, also known as MTX, is a drug that frequently fails because it doesn’t always accumulate correctly at the site of implantation, a problem that polymersomes aim to solve.
By preventing embryonic cells from proliferating, MTX prevents ectopic pregnancy. However, even when it is effective, MTX can have a number of side effects for the patient, including nausea, vomiting, diarrhea, raised liver enzymes, kidney damage, and lung illness.
“A lower dose,” the scientists say, “would be a step in the right direction for reducing side effects as well as increasing efficacy.”
Two percent of all pregnancies in the United States, and between 1% and 2% worldwide, are ectopic, the authors note. In the U.S. alone that translates to approximately 100,000 ectopic pregnancies annually.
The fallopian tubes are the site of almost 98% of ectopic implantations, putting women at risk for hemorrhaging and death.
A dose of MTX delivered by polymersomes induced the end of pregnancy in mice, whereas the same dose of MTX by itself didn’t. To achieve the same therapeutic efficacy with MTX alone, we had to increase the dosage sixfold. Also very promising is that, after having pregnancies ended by MTX-loaded polymersomes, mice successfully conceived and gave birth to healthy offspring.
Olena Taratula
“Developing drugs able to target specific locations in the body remains one of biomedicine’s greatest challenges,” Taratula said. “Most of the drugs prescribed today, including MTX, have no means of working only on specific tissues or cells. When drugs affect healthy cells, it can drastically reduce a patient’s quality of life think of the severe effects of chemotherapy like hair, loss of the lining of the gut, ulcer formation, nausea, etc.”
Taratula, Baldwin and other researchers at OHSU and the Oregon State College of Pharmacy sought to reduce MTX’s shortcomings by exploring whether packaging it in a special type of nanoparticle, polymersomes, would enable the drug to target only embryonic cells.
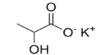
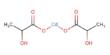
Hollow spheres known as polymersomes are man-made counterparts of liposomes, which are lipid-based sacs present in all living cells. Loading MTX into polymersomes prevents it from acting until the glutathione prompts its release; the scientists created a polymersome that would react to the high amounts of a chemical known as glutathione in placental cells.
“A dose of MTX delivered by polymersomes induced the end of pregnancy in mice, whereas the same dose of MTX by itself didn’t,” Taratula said. “To achieve the same therapeutic efficacy with MTX alone, we had to increase the dosage sixfold. Also very promising is that, after having pregnancies ended by MTX-loaded polymersomes, mice successfully conceived and gave birth to healthy offspring.”
Collaborators on the study included Babak Mamnoon, Abraham Moses, Constanze Raitmayr and Oleh Taratula of the OSU College of Pharmacy and Terry Morgan of OHSU.
In addition, Taratula is continuing her investigation on the use of different kinds of nanoparticles to identify and terminate ectopic pregnancy. She headed a team that created a light-sensitive nanoparticle for those uses a year ago.
She said that since a magnetic field may penetrate tissue more deeply than light, they may be even more effective than the light-sensitive nanoparticles.