Researchers discovered never-before-seen genetic alterations and a more precise method to study the IRAK4 gene responsible for innate immunity as a result of an infant’s peculiar instance of a rare encephalitis not commonly encountered in children.
The IRAK4 gene directs the creation of a protein that is essential for the early detection and defense against pathogen invasion. An immune system problem brought on by inherited abnormalities in this gene can make the body vulnerable to repeated infections with pus-forming pyogenic bacteria.
Cases of IRAK4 deficiency are quite rare and only about 10 familial instances were identified so far in Japan.
A Hiroshima University-led research team detected two novel IRAK4 mutations, c.29_30delAT (p.Y10Cfs*9) and c.35G>C (p.R12P), in a 10-month-old boy with anti-N-methyl-d-aspartate receptor (anti-NMDAR) encephalitis and human herpesvirus 6 (HHV6) reactivation.
The p.Y10Cfs*9 and p.R12P variations were inherited from his father and mother, respectively. The research team found the mutations by using whole exome sequencing (WES), a method used to exhaustively examine the DNA for genetic disorders.
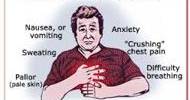
When the immune system targets a crucial brain receptor, anti-NMDAR encephalitis, an inflammation of the brain, results, resulting in mental symptoms, uncontrollable movement, convulsions, autonomic dysfunction, and central hypoventilation. It usually happens to older females with ovarian tumors. Only a few cases of anti-NMDAR encephalitis have been so far reported in infants.
It is well known that anti-NMDAR encephalitis is triggered by HSV1 (herpes simplex virus) infection. The post-infectious autoimmune process that follows the HSV-induced brain damage is thought to be the cause of anti-NMDAR encephalitis.
The researchers
The researchers suspect that reactivation of HHV6 may have induced brain damage that triggered the production of anti-NMDAR antibodies.
“It is well known that anti-NMDAR encephalitis is triggered by HSV1 (herpes simplex virus) infection. The post-infectious autoimmune process that follows the HSV-induced brain damage is thought to be the cause of anti-NMDAR encephalitis,” the researchers said in their study published in the Journal of Clinical Immunology.
“The coexistence of anti-NMDAR encephalitis and HHV6 reactivation in this patient may reveal an unknown manifestation associated with IRAK4 deficiency,” they said.
More precise method to analyze IRAK4 mutations
Although the researchers have yet to find direct evidence demonstrating a relationship between IRAK4 deficiency and the development of anti-NMDAR encephalitis or HHV6 reactivation, they were able to establish that mutations p.Y10Cfs*9 and p.R12P are damaging.
The researchers developed a novel NF-κB reporter assay that can precisely evaluate whether an IRAK4 mutation is harmful. The reporter assay allows them to investigate the activation of transcription factor NF-κB which regulates the body’s inflammatory responses.
“Using this system, we confirmed that both novel mutations are deleterious. The current case revealed the possibility that genetics can contribute to characterizing infantile cases with anti-NMDAR encephalitis,” study author Satoshi Okada, a professor at HU’s Graduate School of Biomedical and Health Sciences, said.
By employing CRISPR gene-editing technology to delete the IRAK4 naturally produced in the HEK293 cell, which is frequently employed in studying gene function since it is much easier to transfect than other cell lines, they were able to resolve potential difficulties of misevaluation in a previously published NF-κB reporter assay.
“HEK293 cells have endogenous IRAK4 expression. Their endogenous IRAK4 prevents the precise evaluation of the activity of introduced WT or mutant IRAK4,” Okada explained.
To date, there are so far 24 known mutations identified in patients with IRAK4 deficiency. The study team anticipates releasing their brand-new NF-κB reporter assay system in the near future to aid in assessing IRAK4 gene alterations and achieving early diagnosis.