Diagnostic Ultrasonography is an established, effective imaging technique, which employs the use of ultrasound waves for imaging. It is a relatively inexpensive, fast, and noninvasive and radiation free imaging modality. High frequency (7.5 to 10.0 MHz) probes emit sound waves that attenuate rapidly with increasing depth (Mclvor et al.1993). The normally homogenous texture of thyroid, it’s clearly defined surrounding structures and its relatively superficial location makes it is an ideal structure for evaluation by high frequency ultrasonography.
Thyroid gland is affected by pathological lesion of various morphology, which can be divided into two types, diffuse and nodules. The nodular lesions comprise disorders that consist of neoplastic nodules as well as benign and malignant (Livolsi, 1997).
Patients presenting with a palpable thyroid nodule is a common clinical dilemma (Wong and Ahuja, 2005). Any thyroid disease can appear as one or more thyroid nodules, but the differential diagnosis embraces chiefly the disorders. Of nodules removed surgically, an estimated 42 to 77 % are non neoplastic colloid nodules, 15 to 40 % are adenomas, and 8 to 17 % are carcinoma (Mazzaferri, 1993). The incidence of solitary thyroid nodule is approximately 3.2% of the population in the UK and 4.2% in the USA (Wong and Ahuja, 2005; Tunbridge et al.1977; Rojeski and Gharib 1985).The risk of malignancy in a euthyroid patient with a solitary nodule is estimated to be 5% to 10% with a range of 3.4% to 29% (Wong and Ahuja, 2005; Rojeski and Gharib 1985). Most of the thyroid nodules are benign, but 4-14% of such nodules are malignant (Yoon et al. 2007). Thus, it is important to identify which nodules are more likely to be malignant.
Although thyroid nodules are traditionally found as palpable masses at neck examination in patients with or without suspected thyroid disease, the apparent prevalence of non-palpable thyroid nodules (i.e. <1cm ) in the general population has recently increased, probably as a consequence of the increasing application of ultrasound (Cappelli et al. 2006)
There is a set of ultrasonographic characteristics that identify nodules at higher risk of malignancy. These are presence of microcalcification within a nodule, blurred margin, hypoechoic pattern, intranodular vascular flow (Cappelli et al. 2006), the absence of a halo and a predominantly solid composition (Yoon et al. 2007)
The major roles of ultrasound include: detection and characterization of thyroid cancer; detection of cervical nodal metastasis; follow-up of patients after treatment for early detection of local or nodal tumor recurrence; and provide imaging guidance for FNAC or biopsy (Cappelli et al. 2006).
High frequency transducers allow superior near field resolution and form the basis of characterization of benign and malignant thyroid nodules (Wong and Ahuja, 2005; Mazzaferri, 1993). FNAC is inexpensive, widely available and easy to perform, and is therefore regarded as a part of the initial investigation for a thyroid nodule. It has a pre-operative predictive accuracy of more than 90% and aids the surgeon in selecting the most appropriate procedure prior to surgery (Wong and Ahuja, 2005; Rojeski and Gharib, 1985).
This study will be conducted to evaluate the roll of ultrasound in detection of carcinoma of thyroid . The study is based on the presumption that an accurate diagnosis helps to reduce high negative thyroidectomy rates and thereby benefit affected patients.
Rationale
The prevalence of palpable thyroid nodules increases with age and it is four times more common in women than in men. A nodule raises concerns about malignant disease. Solitary nodules are more common than multinodular goiters clinically, and solitary nodules considered more likely to harbor malignant disease. Clinical examination is poor at detecting small thyroid nodules. Early aggressive treatment and unnecessary investigation and surgery can be avoided in the majority of patients who have a benign nodule. High resolution ultrasound helps to differentiate a malignant nodule from a more common benign thyroid nodule and identify a malignant nodule against a background nodular goiter. In most centers, ultrasound with FNAC is the initial investigation of choice. The main aim of any imaging investigation is to identify accurately those patients with malignant thyroid nodules so that appropriate treatment can be offered.
In our country it is also a common medical problem but unfortunately there is limited research work in this field in Bangladesh and it is very important to do this research work like the developed countries. As for this purpose, if my hypothesis is tested, it can help in diagnosis and management of thyroid diseases having malignant nodules of our population by using our own data.
Hypothesis
“Ultrasonography is an important diagnostic tool for detection of thyroid carcinoma.”
Objectives
General objective:
- To determine the roll of ultrasonography in the diagnosis of thyroid carcinoma.
Specific objectives:
- To observe the nature of the thyroid carcinoma by ultrasonography.
- To compare the findings of ultrasonography with that of histopatholgy.
- To observe sensitivity, specificity, positive predictive value, negative predictive value and accuracy of ultrasonography in patients with thyroid carcinoma.
Related previous studies
Baier et al. (2009) retrospective studies determine the likelihood of malignancy in thyroid nodules and the risk of a nondiagnostic fine – needle aspiration biopsy (FNAB) on the basis of the demographic features of the nodules. In their study they included adult patients who underwent thyroid nodule FNAB and had previously undergone diagnostic sonography. From previous reports for 944 thyroid nodules (739 nodules in women and 205 nodules in men), four sonographic features were recorded: longest dimension, morphology, presence of microcalcifications and presence of limphadenopathy. Final diagnosis of each nodule was classified as benign, malignant or nondiagnostic on the basis of surgical pathology when available and cytology otherwise and was analyzed for correlation with individual sonographic features and combinations of features. The prevalence of malignancy and of nondiagnostic FNAB in this study was 11.0% and 11.8%, respectively. Statistically significant (p< 0.05) findings in malignanat nodules were younger patients age (≤45 years; odds ratio [OR], 1.54) and solid nodule morphology ( OR, 2.38). The significant predictors of a nondiagnostic- quality FNAB were older patient age ( >75 years; OR, 1.95) and a nodule ≥10mm (OR, 1.45). Adding information about the other evaluated ultrasound features did not lead to a significant result. They concluded that the malignant thyroid nodules tend to be solid (86.5). Patients older than 75 years showed a clearly increased risk of nondiagnostic FNAB, but to predict a higher risk of malignancy or of nondiagnostic FNAB using ultrasound remain difficult.
Binesh and Salari (2008) was conducted a study to determine the accuracy of fine-needle aspiration biopsy diagnosis. During their cross-sectional study, reports of 600 fine needle aspiration cytology of the thyroid performed during a period of 11 years (1991-2001), pathological diagnosis were available for 28 cases. Cytological reports were classified diagnostically, and histological and cytological correlations were determined. Statistical analysis was performed with SPSS 13 and descriptive test. From 600 cases (91 male, 509 female) the cytological diagnosis were as follows: 526 (87.7%) benign, 28 (4.7%) malignant, 10 (1.6%) suspicious and 36 (6%) unsatisfactory. Between benign lesion, goiter and follicular adenoma and between malignant lesions, papillary cell carcinomas were the most common. Malignant nodules were more common in females than males (4.9% versus 3.3%). We identified no false-positive results between malignant FNA and histopathology and so positive predictive value was 100%. They concluded that fine-needle aspiration of the thyroid gland is highly accurate and has a low rate of false-positive diagnosis in case of malignant results.
Yoon et al. (2007) in a study retrospectively analyzed the ultrasonographic features of 65 pathologically proven thyroid lesions showing peripheral calcification for their correlation with histopathological results. The following ultrasonographic parameters were assessed for each nodule: size (maximal dimension), shape (anteroposterior dimension/transverse dimension ratio), internal echogenicity (hypoechoic, isoechoic, hyperechoic or invisible), and halo sign (present or absent), type of calcification (stippled, curvilinear/smooth margin, or curvilinear/irregular margin), and extend of calcification (arc or rim). Twelve (18.5%) of thyroid nodules with peripheral calcification were malignant, and 53 (81.5%) were benign. Patient demographics (age and sex) and ultrasonographic features of the nodules (size, shape, internal echogenicity, halo sign and type and extend of calcification) did not show any significant differences between benign and malignant groups. They concluded that the relatively high prevalence of malignancy and no reliable criterion for malignancy in thyroid nodules with peripheral calcification indicate that fine-needle aspiration or careful ultrasonographic follow up may be warranted in these cases.
Cappelli et al. (2006) in a prospective observational study evaluated whether ultrasonographic features of thyroid nodules are associated with histological malignancy and to identify useful criteria for clinical decision-making. Overall, 7455 nodules (diameters from 6 to 100 mm) were examined: 2865 (38.4%) were <10 mm in diameter. All patients with suspicious or malignant cytology underwent surgery. Of the 349 nodules undergoing surgery, 284 were malignant. The prevalence of cancer was slightly higher in nodules ≥ 10 mm in diameter vs. those < 10 mm (5.5% vs. 3.0%, p< 0.001). However, histological type and local aggressiveness were largely independent of nodule size. Micro calcifications (72.2% vs. 28.7%; p < 0001) , blurred margins (52.8% vs. 18.8%; p < 0001), solid hypoechoic appearance (80.6% vs. 52.4%; p < 0001), size ≥ 10 mm (77.4% vs. 64.9%; p < 0001) and intranodular vascular pattern type 2 (61.6% vs. 49.7%; p < 0001) were all significantly more frequent in malignant than in benign nodules. These associations were similar when large and small nodules were analyzed separately. They concluded that no single parameter, including nodule size, satisfactorily identifies a subset of patients to be electively investigated by FNAC, although several may be useful in this regard.
Thapa (2004) showed 100 percent sensitive and 91 percent specific for the diagnosis of benign thyroid nodules with positive predictive value (PPV) of 97 percent and negative predictive value (NPV) of 100 percent (p = 0.01). For the diagnosis of the malignant thyroid nodule USG is 91 percent sensitive and 100 percent specific with PPV of 100 percent and NPV of 97 percent (p= 0.001). Similarly the USG diagnosis was 100 percent sensitive and 81 percent and NPV of 100 percent (p = 0.0003). He concluded that USG is a sensitive and specific imaging modality in the diagnosis work up of patients with neck masses.
In Takashima et al. (1995) study diagnosis accuracy of micro calcification and other various signs seen in USG scans for predicting malignancy was evaluated prospectively in 259 pathologically verified thyroid nodules. Sonographic and pathologic correlation of calcification was performed on 69 of 99 surgically removed nodules. Pathologic studies revealed that hyperechoic areas with acoustic shadowing represented mostly amorphous dense calcifications and sometimes microcalcifications, but small particles without acoustic shadowing mainly reflected micro calcifications and sometimes large amount of fibrous bands and condensed colloids. Of the various sonographic signs, microcalcification showed the highest accuracy (76%), specificity (93%) and positive predictive value (70%) for malignancy as a single sonographic sign, but its sensitivity (36%) was poor. Although sonographic microcalcificatin showed relatively high specificity, the accuracy of this finding for malignancy was insufficient.
Anatomical Consideration
There are certain organs which are very similar to secreting glands, but differ from them in one essential particular, viz., they do not possess any ducts by which their secretion is discharged. These organs are known as ductless glands. Thyroid is one of the important ductless glands of body (Williams et al. 1995). Thyroid is an endocrine gland, situated in the lower part of the front and sides of the neck. It regulates basal metabolic rate, stimulates somatic and psychic growths, and plays important role in calcium metabolism (Chaurasia, 2004). The thyroid gland is a highly vascular organ, situated at the front and sides of the neck; it consists of right and left lobs connected across the middle line by a narrow portion, the isthmus. Its weight is somewhat variable, but is usually about 30 grams. It is slightly heavier in the female, in whom it becomes enlarged during menstruation and pregnancy (Williams et al. 1995).
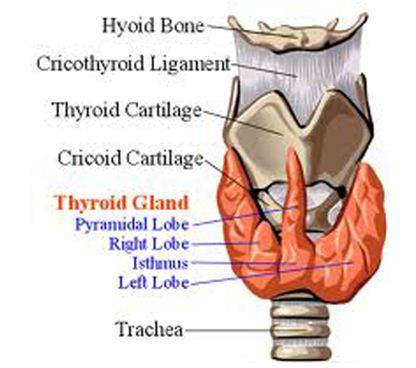
Figure: Normal structure of thyroid gland
Shape:
It is roughly H-shaped; the vertical limbs represent two lobes and the horizontal limbs, isthmus (Chaurasia, 2004).
Situation and extent:
The thyroid gland is a highly vascular organ, situated at the front and sides of the neck:
- The gland lies against C5-7 and T1 vertebrae
- Each lobe extends from middle of the thyroid cartilage to the fourth or fifth tracheal ring (Chaurasia, 2004).
Parts of the thyroid gland:
It consists of right and left connected across the middle line by a narrow portion, the isthmus. A third, pyramidal lobe is often present (Chaurasia, 2004).
The lobes are conical in shape having:
- Apex
- Base
- Three surfaces, lateral , medical and posterolateral and
- Two borders, anterior and posterior
The apex of each being directed upward and slightly laterally as far as the junction of the middle with the lower third of the thyroid cartilage: the base looks downward and is on a level with the fifth or tracheal ring (Chaurasia, 2004).
The lobes (lobuli gl. Thyreoidea) are conical in shape, the apex of each being directed upward and lateralward as far as the junction of the middle with the lower third of the thyroid cartilage; the base looks downward and is on a level with the fifth or sixth tracheal ring. Each lobe is about 5 cm. long; its greatest width is about 3 cm and its thickness about 2 cm. The lateral or superficial surface is convex and covered by the skin, the superficial and deep fascia, the Sternocleidomastoid, the superior belly of the Omohyoid, the Sternohyoid and beneath the last muscle by the pretracheal layer of the deep fascia, which forms a capsule for the gland. The deep or medial surface is moulded over the underlying structures, viz., the thyroid and criciod cartilages, the trachea, the Constrictor pharyngis inferior and posterior part of the Cricothyroid, the oesophagus (particularly on the left side of the neck), the anterior border is thin and inclines obliquely from above downward toward the middle line of the neck, while the posterior border is thick and overlaps the common carotid artery and as a rule, the parathyroids (Williams et al. 1995).
The isthmus (isthmus gl. thyreoidea) connects together the lower thirds of the lobes; it measures about 1.25 cm in breadth, and the same in depth, and usually covers the second and third rings of the trachea. Its situation and size present, however, many variations. In the middle line of the neck it is covered by the skin and fascia, and close to the middle line, on either side, by the Sternothyreoideus. Across its upper border runs an anastomotic branch uniting the two superior thyroid arteries; at its lower border are the inferior thyroid veins (Williams et al.1995).
A third lobe, of conical shape, called the pyramidal lobe ,frequently arises from the upper part of the isthmus ,or from the adjacent portion of either lobe, but most commonly the left, and ascends as far as the hyoid bone. It is occasionally quite detached, or may be divided into two or more parts. A fibrous or muscular band is sometimes found attached, above, to the body of the hyoid bone, and below to the isthmus of the gland, or its pyramidal lobe. When muscular, it is termed the Levator glandulae thyreoideae. Small detached portions of thyroid tissue are sometimes found in the vicinity of the lateral lobes or above the isthmus; they are called accessory thyroid glands ( glandulae thyreideae accessoriae) (Williams et al.1995).
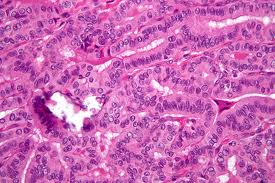
Structure of the thyroid gland:
The thyroid gland is invested by a thin capsule of connective tissue, which projects into its substance and imperfectly divides it into masses of irregular from and size .When the organ is cut into, it is of a brownish-red color, and is seen to be made up of a number of closed vesicles, containing a yellow glairy fluid, and separated from each other by intermediate connective tissue(Williams et al.1995).The vesicles of the thyroid of the adult animals are generally closed spherical sacs; but in some young animals, e.g., young dogs, the vesicles are more or less tubular and branched. This appearance is supposed to be due to the mode of growth of the gland, and merely indicates that an increase in the number of vesicles is taking place. Each vesicle is lined by a single layer of cubical epithelium. There does not appear to be a basement membrane, so that epithelial cells are in direct contact with the connective-tissue reticulum which supports the acini. The vesicles are of various sizes and shapes, and contain as a normal product a viscid, homogeneous, semifluid, slightly yellowish, colloid material; red corpuscles are found in it in it in various stages of disintegration and decolorization, the yellow tinge being probably due to the haemoglobin, which is set free from the colored corpuscles. The colloid material contains an iodine compound, iodothyrin, and is readily stained by eosin. According to Bensley the thyroid gland prepares and into the vascular channels a substance, formed under normal conditions in the outer pole of the cell and excreted from it directly without passing by the indirect route through the follicular cavity. In addition to this direct mode of the secretion there is an indirect mode which consists in the condensation of the secretion into the form of droplets, having high content of solids, and the extension of these droplets into the follicular cavity. These droplets are formed in the same zone of the cell as that in which the primarily or direct secretion is formed (Williams et al.1995).
Vessels and Nerves of the thyroid gland:
The arteries supplying the thyroid gland are the superior and inferior thyroids and sometimes an additional branch (thyroidea ima) from the innominate artery or the arch aorta, which ascends upon the front of the trachea. The arteries are remarkable for their large size and frequent anastomoses. The veins from a plexus on the surface of the gland and on the front of the trachea; from this plexus the superior, middle, and inferior, and inferior thyroid veins arise; the superior, middle end in the internal jugular , the inferior in the innominate vein. The capillary blood vessels from a dense plexus in the connective tissue around the vesicles, between the epithelium of the vesicles and the endothelium of the lymphatics, which surround a greater or smaller part of the circumference of the vesicle. The lymphatic vessels run in the interlobular connective tissue, not uncommonly surrounding the arteries which they accompany, and communicate with a net-work in the capsule of the gland; they may contain colloid material. They end in the thoracic and right lymphatic trunks. The nerves are derived from the middle and inferior cervical ganglia of the sympathetic (Williams et al.1995).
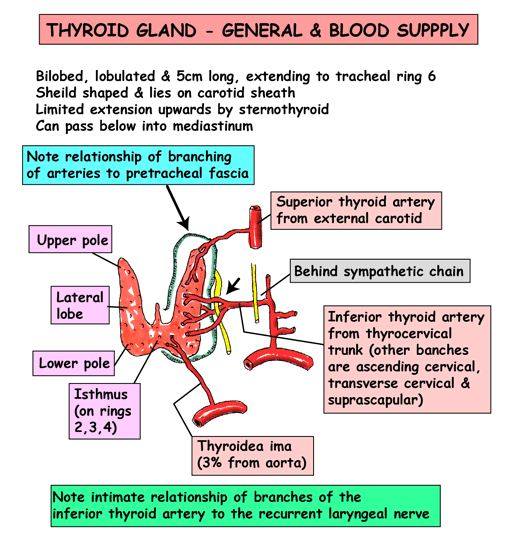
Figure- Vascular supply of thyroid gland
Development of thyroid gland:
The thyroid gland is developed from a median diverticulum, which appears about the fourth week on the summit of the tuberculum impar, but later is found in the furrow immediately behind the tuberculum. It grows downward and backward as a tubular duct, which bifurcates and subsequently subdivides into a series of cellular cords, from which the isthmus and lateral lobes of the thyroid gland are developed. The ultimo-branchial bodies from the fifth pharyngeal pouches are enveloped by the lateral lobes of the thyroid gland; they undergo atrophy and do not form true thyroid tissue. The connection of the diverticulum with the pharynx is termed the thyroglossal duct; its continuity is subsequently interrupted, and it undergoes degeneration, its upper end being represented by the foramen cecum of the tongue, and its lower by the pyramidal lobe of the thyroid gland (Williams et al.1995).
Pathological Consideration:
Thyroid nodule:
A thyroid nodule is a palpable swelling in a thyroid gland with an otherwise normal appearance. Thyroid nodules are common and may be caused by a variety of thyroid disorders. While most are benign, about 5 percent of all palpable nodules are malignant (Mazzaferri 1992; Gharib and Goellner 1993; Giuffrida and Gharib 1995; Castro and Gharib 2000).Many tests and procedures are available for evaluating thyroid nodules, and appropriate selection f tests is important for accurate diagnosis. Family physicians should have a cost-effective method of differentiating between nodules that are malignant and those that will have a benign course. This article provides a method for the outpatient evaluation and treatment of thyroid nodules.
Presentation:
The majority of thyroid nodules are asymptomatic. Most persons with thyroid nodules are euthyroid, with less than1 percent of nodules causing hyperthyroidism or thyrotoxicosis. Patients may complain of neck pressure or pain if spontaneous hemorrhage into the nodule has occurred. Questions about symptoms of hypothyroidism or hyperthyroidism are essential, as are questions about any nodule, goiter, family history of autoimmune thyroid disease (e.g.,Hashimoto’s thyroiditis, Graves’ disease), thyroid carcinoma or familial polyposis (Gardner’ syndrome).
Colloid nodules are the most common and do not have an increased risk of malignancy. Most follicular adenomas are benign; however, some may share features of follicular carcinoma. About 5 percent of microfollicular adenomas prove to be follicular cancers with careful study (Mazzaferri, 1992). Thyroiditis also may present as a nodule (figure 5).Thyroid carcinoma usually presents as a solitary palpable thyroid nodule. The most common type of malignant thyroid nodule is papillary carcinoma
Types of Thyroid Nodules:
Adenoma
- Macrofollicular adenoma (simple colloid)
- Microfollicular adenoma (fetal)
- Embryonal adenoma (trabecular)
- Hurthle cell adenoma (oxyphilic, onococytic)
- Atypical adenoma
- Adenoma with papillae
- Signet-ring adenoma
Carcinoma
- Papillary (75 percent)
- Follicular (10 percent)
- Medullary (5 to 10 percent)
- Anaplastic (5 percent)
- Other
- Thyroid lymphoma (5 percent)
Cyst
- Simple cyst
- Cystic/solid tumors(hemorrhagic,necrotic)
- Colloid nodule
- Dominant nodule in a multinodular goiter
Other
- Infalmmatory thyroid disorders
- Subcute thyroiditis
- Chronic lymphocytic thyroiditis
- Granulomatous disease
- Developmental abnormalities
- Dermoid
- Rare unilateral lobe agenesis (Mazzaferri 1993)
Ultrasonography of the thyroid gland:
Ultrasound examination of thyroid gland and the neck region is basic diagnostic imaging method providing information on structure of parenchyma of the thyroid gland, on its relationship to its surroundings and on regional lymphnodes (Martineka, et al. 2004).
This is a multidisciplinary and involves head and neck surgeons, pathologists and radiologists. Ultrasound is easy to perform, widely available, does not involve management of thyroid nodule ionizing radiation. It is therefore an ideal investigation of choice for evaluating thyroid nodules. It evaluates specific features that help in identifying the nature of the nodule. The use of high frequency transducers has significantly improved the spatial and contrast resolution in evaluating superficial structures including the thyroid gland. One obvious advantage of ultrasound over other imaging modality is to combined with histopathology to increase the diagnostic accuracy.
Ultrasound examination of the thyroid must always include a detailed examination of the neck any cervical lymhphadenopahy. Metastatic cervical lymphnodes are seen in thyroid cancer and may affect the surgical management and prognosis of patients. The vast majority of thyroid nodules are benign, and the role of a radiologist in assessment of the thyroid gland is top differentiate a malignant thyroid nodule from the more commonly seen benign ones. It is therefore important to evaluate the sonographic features of the thyroid nodules as this aid in their characterization.
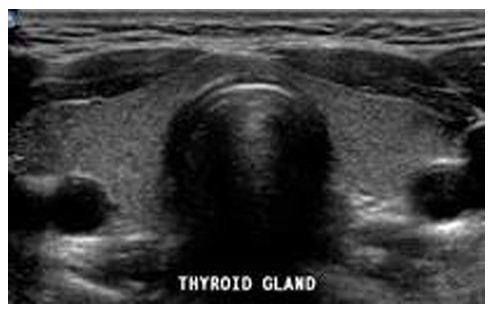
Figure: Sonographic appearance of normal thyroid gland
Echogenicity
The incidence of malignancy is 4% when a solid thyroid nodule is hyperechoic. If the lesion is hypo echoic, the incidence of malignancy rises to 26%.However, hypoechogenicity alone is inaccurate in predicting malignancy, and if used as sole predictive sign, it has a sole predictive sign; it has a relatively poor specificity (49%) and positive predictive value (40%).
Margins and halo sign
A malignant thyroid nodule tends to have ill-defined margins on ultrasound.
A peripheral halo of decreased echogenicity is seen around hypoechoic and isoechoic nodules and is caused by either the capsule of the nodule or compressed thyroid tissue and vessels. The absence of a halo has specificity of 77% and sensitivity of 67% in predicting malignancy.
Calcification
Fine punctate calcification due to calcified psammoma bodies within the nodule is seen in papillary in 25 % to 40 % of cases. If used as a sole predictive sign of malignancy, microcalcification is the most reliable one with accuracy of 76 %, specificity of 93% and a positive predictive value of 70 % coarse, dysmorphic, curvilinear calcifications commonly indicate benignity.
Comet tail sign
Presence of a comet tail sign in a thyroid nodule indicates the presence of colloid within a benign nodule and is a strong predictor of benignity.
Solid/cystic
It is generally believed that thyroid nodules with large cystic components are usually benign nodules that have undergone cystic degeneration or hemorrhage. However, papillary carcinoma occasionally demonstrates a cystic component and may mimic a benign nodule, through the presence of punctate calcification within the component helps in its identification
Multinodularity
It is a myth that multinodularity implies benignity, as approximately 10%-20% of papillary carcinomas may be multicentric. In those with true solitary nodules confirmed at surgery the risk of cancer is as the same as in those with multinodular goiters. Therefore against a background of multinodular changes, extra caution should be taken not to miss a suspicious nodule (Wong and Anil, 2005).
Ultrasound characteristics which suggest a benign nodule
- Nice sharp edges are seen all around the nodule
- Nodule filled with fluid and not live tissue(a cyst)
- Lots of nodules throughout the thyroid(almost always a benign multinodular goiter)
- No blood flowing through it(not live tissue, likely a cyst)
Ultrasound characteristics which suggest a malignant nodule
- Predominantly solid(70%) and hypoechoic (77%-90%)
- Presence of punctate microcalcification (25%-90%) correspond to psammomas bodies on microscopy.
- Ill –defined margins
- Areas of necrosis in 78%
- Nodal or distant metastases in 80% of patients [45, 46]; the involved lymph nodes show evidence of necrosis in 50%>
- Extra capsular spread and vascular invasion in a third of patients (Wong and Anil, 2005).
Limitation of the thyroid ultrasound
Ultrasound, in most cases, cannot accurately distinguish a benign from malignant follicular lesion. The suspicion of malignancy is raised if the nodule is ill-defined, hypoechoic, has a thick irregular capsule and chaotic intranodular vascularity. The only reliable signs of malignancy on ultrasound include frank vascular invasion to adjacent vessels (such as internal jugular vein and common carotid artery) and extracapsular spread (Wong and Anil, 2005).
Research approach
This cross sectional study was carried on consecutively selected 52 patients aged 15-60 years admitted in ENT indoor and also from ENT outdoor and other department of DhakaMedicalCollege for discrimination of benign and malignant nodules by ultrasonography before surgical intervention. Initially a total of 60 patients with thyroid swellings were registered for screening for high resolution sonography. But with the course of the time 10 patients were excluded from the study as a dropout case or refused to co-operative for further with the study. Among them 41 were female and 11 were male. After informed written consent, ultrasonogram was performed first by the investigator which then subsequently confirmed by a radiologist of the department of Radiology & Imaging, Dhaka Medical College separately to eliminate bias. By studding the morphological pattern of the lesion the thyroid nodules were discriminated as benign or malignant before surgical intervention. Tissues of surgically removed nodules were sent to the respective pathology department for histopathological diagnosis. All findings of clinical examination, history and ultrasonography were recorded in a pre-designed data collection sheet.
Study design:
This was a cross-sectional study.
Duration of the study:
Study period was one year, starting from January 2012 to December 2012.
Place of study:
The study was carried out in the department of Radiology and Imaging, DhakaMedicalCollegeHospital.
Ethical consideration:
Prior to the commencement of this study the research protocol was approved by Local ethical committee (RRC & EC) of DhakaMedicalCollege, Dhaka. The objectives of this study along with its procedure risks and benefit were fully explained to the subjects in easily understandable local language and then informed written consent was taken from each patient. It was assured that all information and records would be kept confidential and the procedure would be helpful for both the surgeon and the patient in making rational approach of the case management.
Criteria for selection of the patients
Inclusion criteria:
- Patients with clinically suspected thyroid carcinoma:
-palpable normal thyroid gland.
-enlarged cervical node.
- Cytologically or histopathologically diagnosed of the disease.
Exclusion criteria:
- Non availability of histopathological reports.
- Patients who refused surgery.
Sample size:
It is determined by the following formula-
Where,
n = the desired sample size.
z = the standard normal deviate, usually set at 1. 96 at 5% level which corresponds to 95% confidence level.
P = the assumed target proportion. q = 1-p, here p = 0.50
d = is the degree accuracy level considered as 5%. The degree of accuracy d, which assume, is 0.05.
Putting the value in the above equation the sample size, n estimates as –
3.84x 0.5 x 0.5
———————
0.052
n= 384 (targeted sample size)
It is observed that 6 patients fulfill the inclusion criteria in one month. The total duration of the study is 12 months and the population size is roughly estimated 72. If N is less than 10,000 then the required sample size will be much smaller which is calculated by the following formula-
nf = the desired sample size, when population is less than 10,000.
n = the desired sample size, when population is more than 10,000.
N= the estimate of population size
According to this formula, the estimated final sample size is going to be 52.
Variables
The following variables were included:
A. Demographic variables
- Age
- Sex
B. Sonographic variables
- Margin
- Shape
- Halo sign
- Echostructure
- Echogenicity
- Calcification
- Invasion to adjacent organs
- Cervical lymphadenopathy
C. Statistical variable
- Sensitivity
- Specificity
- Positive predictive value
- Negative predictive value
- Accuracy
Scanning technique:
Proper counseling and reassurance to the patient regarding the examination procedure was done to reduce their apprehension and to get full cooperation. Informed consent was taken from each of the patient.
Ultrasonogrphy of the thyroid gland was done with 7.5 MHz probe. High frequency transducer is the basic equipment and it allow superior near field resolution and formed the basis of characterization of benign and malignant thyroid nodules (Wrong and Anil 2005). The patient was placed in supine position with extended neck. Pillow was placed under the neck to ensure adequate exposure of the gland. Examination was started from lateral side of neck, landmark used are external carotid artery and jugular vein. Both longitudinal and transverse sections were taken. After localizing the nodule following features were noted.
The fundamental anatomic features of a thyroid nodule on high-resolution sonography are:
- Internal consistency (solid, mixed solid and cystic or purely cystic)
- Echogenicity relative to the adjacent thyroid parenchyma
- Margin
- Presence and pattern of calcification
- Peripheral sonolucent halo
- Presence and distribution of blood flow signals
Data collection
Written consent was taken from all the patients regarding the research study. The data were collected in a pre-designed structured data collection sheets (proforma) as mentioned in Appendix II.
Data analysis
Statistical analysis of the results was done by computer software devised as the statistical package for the social sciences (SPSS).The results were presented in tables, figures, and diagrams. For the validity of the study outcome sensitivity, specificity, accuracy, positive and negative predictive values of USG in the diagnosis of thyroid carcinoma was calculated out after confirmation of the diagnosis by histopathology. Confidence interval was considered at 95% level.
OBSERVATIONS AND RESULT
The present study was conducted to evaluate the role of USG in the diagnosis of carcinoma of thyroid gland with histopathological correlation in the department of Radiology and Imaging of Dhaka medical College, Dhaka. Total 52 patients with thyroid pathology were included in the present study. The results of the present study as followed:
Table : Mean age distribution of the of the study subjects (n=52)
| Age (in year) | Frequency | Percent | Mean ± SD |
| 15-25 | 15 | 28.8 | 32.26 ± 9.01 |
| 25-45 | 35 | 67.3 | |
| 45-60 | 2 | 3.8 | |
| Total | 52 | 100.0 |
Table showed the distribution of the respondents by age. Total 52 respondents were grouped in 3 groups, ranging from 15-25, 25-45 and 45-60 yrs. Mean (±SD) age of the study group was 32.26 (±9.01) and range was 15-60 years. Highest number of patients was in the age group of 25-45 and lowest number was in age group above 45 years.
Table : Sex distribution of the study subjects (n=52)
| Sex | Frequency | Percent |
| Male | 11 | 21.2 |
| Female | 41 | 78.8 |
| Total | 52 | 100.0 |
Male: Female =1:3.73
Table showed the distribution of the respondents by sex. Out of the respondents 74.1% were female, rest 25.9% were male. The ratio between male and female of the study groups was 1:3.73.
Table : Distribution of the study subjects according to ultrasound findings of the thyroid gland (n=52)
| Ultrasound finding | Frequency | Percent |
Number of nodule
| 45 7 | 86.5 13.5 |
Position of nodule
| 31 17 4 | 59.6 32.7 7.7 |
Margins of nodule
| 35 17 | 67.3 32.7 |
| Irregular shape | 15 | 28.8 |
Echo structure
| 19 2 21 | 36.5 3.8 40.4 |
Echogenicity
| 3 4 3 | 6.0 7.7 6.0 |
| Calcification | 32 | 59.3 |
| Absence of Halo | 17 | 35.2 |
| Cervical lymphadenopathy | 3 | 5.8 |
| Adjacent structure involvement | 2 | 3.8 |
Table shows the distribution of ultrasound finding of the thyroid gland. Findings of ultrasonography of thyroid nodule among the 52 cases was categorized as: number of the nodule (single/ multiple), position of the nodule (right lobe, left lobe and both lobes), size of the nodule (less than 2 cm and 2 cm or more), margins (regular and irregular) and echostructure (solid, cystic and complex mass), echogenicity (echogenic, hypoechoic and heterogenic), cervical lymphadenopathy and adjacent structure involvement. Special features included presence of calcification, halo sign and comet tail sign.
Table No : Distribution of the study subjects according to histopathological findings of thyroid nodule (n=52)
| Histopathological findings | Frequency | Percent |
Benign
| 41 5 3 33 | 78.8 12.1 7.3 80.4 |
Malignant
| 11 8 3 | 21.1 72.7 27.3 |
Table shows the hstopathologic classification of the thyroid nodule. Out of 41 benign tumors 12.1% had follicular adenoma, 7.3% thyroiditis, and 80.4% nodular goiter. Out of 11 malignant tumors 72.7 % papillary & 27.3% had follicular neoplasm.
Table No : Distribution of patients by comparing ultrasound findings and histopathological findings of thyroid nodule (n=52)
| Ultrasonographic findings | Histopathological findings | Total | |
| Malignant | Benign | ||
| Malignant | 10 (TP) | 5 (FP) | 15 |
| Benign | 1 (FN) | 36 (TN) | 37 |
| Total | 11 | 41 | 52 |
TP = True positive; FP= False positive; FN = False negative; TN = True negative.
Out of all cases 15 were diagnosed as having malignant nodule by USG and among them 10 were confirmed by histopathological evaluation. They were true positive. Five cases were diagnosed as having malignant nodule by USG but not confirmed by histopathological findings. They were false positive. Of 37 cases which were confirmed by USG as benign, among them 1 was confirmed as having malignant nodule and 36 were confirm benign by histopathological findings. They were false negative and true negative respectively.
Table No : Validity parameters of ultrasonography for thyroid carcinoma
Value (%) | 95% CI | |
| Sensitivity | 90.9 | 67.4 – 98.3 |
| Specificity | 87.8 | 81.5 – 89.8 |
| PPV | 66.7 | 49.4 – 72.1 |
| NPV | 97.3 | 90.3 – 99.5 |
| Accuracy | 88.5 | 78.5 – 91.6 |
PPV = Positive Predictive Value
NPV = Negative Predictive Value
Sensitivity of USG to diagnose malignant thyroid nodule was 90.9%, specificity 87.8%, positive predictive value 66.7%, negative predictive value 97.3% and accuracy 88.5%.
DISCUSSION
The present study conducted to evaluate the role of USG in the diagnosis of carcinoma of thyroid gland with histopathological correction in the department of Radiology and Imaging of Dhaka Medical College, Dhaka. Total 52 patients with thyroid pathology were included in the present study. The results of the present study as followed:
In the present study total 52 respondents were grouped in 3 groups, ranging from less than 25, 250-045 and above 45 years. Mean (±SD) age of the study group was 32.26 (±9..1) and range was 15 -60 years. Highest number of patients was in the age group of 25 – 45 and lowest number was in age group above 45 years (Table-I). Jen–Der et al. (2007) in their study collected data for 6219 patients with thyroid nodules showed the mean patient age was 49.7 ± 13.9 years and male patients were 45.7 ± 14.9 years.
In the present study out of all respondents 74.1% were female, rest 25.9% were male. The ratio between male and female of the study group was 1:3.73 (Table-II). Hebra et al (2006) in their study found that the thyroid nodules were 2-3 times more common in girls than in boys and comparable with our results.
Findings of ultrasonography of thyroid nodule among the 52 cases was categorized as: number of the nodule (Single/ multiple), position of the nodule (right lobe, left lobe and both lobes), size of the nodule (less than 2 cm and 2cm or more), margins (regular and irregular) and echogenicity (solid, cystic and complex mass, solid with cystic change and hypoechoic). Special features included presence of calcification, halo sign. Carlo et al (2001) in a study showed that out of all cases 77.2% were solitary thyroid nodules and 22.8% were multiple nodules. In Ellen et al. (2000) series ultrasonography revealed 15.7% multinodular, 23.68% nonpalpable, remaining 60.62% solitary nodule. Their study findings comparable with present study.
Among the 11 (100%) malignant cases all were found in single thyroid nodule. None found in multiple thyroid nodules. The 7 were multiple nodules and all were benign cases. Ellen et al. (2000), in a study of 114 cases of solitary nodule, diagnosed by physical for examination, histopathological revealed 7% malignanat, 12% suspicious for malignancy and rest 81% benign. Their results are not similar to present study.
Out of 52 patients adjacent structure involvement present in 17 (32.7%) cases and absent in 35 (67.3%) cases. Relevant literature is not available for compare with these findings.
Out of all patients having benign nodule 85.4% had regular and 14.6% had irregular margin. In malignant nodule all had irregular margin. Thapa (2004) showed that 95 percent of benign nodule was with well defined margin and 90 percent of malignant nodule had poorly defined margin. Their study findings are comparable with present study.
Among the benign cases 41.5% were solid, 4.9% were cystic, 39.0% were complex mass and 14.6% were solid with cystic change. No benign case was found hypoechoic. Among all malignant cases 18.2% were solid, 45.5% were complex mass and 36.4% were hypoechoic. All hypoechoic lesions were malignant. All cystic and solid with cystic change lesion were benign.
Among the 52 respondents, calcification present in 32 (59.3%) case are absent in 20 (40.7%) case in ultrasonographic findings. Among the benign cases in histopathological, calcification present in 22 (51.2%) case and calcification absent in 19 (48.8%) cases. Among the malignant cases 10 (90.9%) were presented with calcification and 1 (9.1%) was presented without calcification.
Out of 52 patients halo sign present in 35 cases and absent in 17 (35.2%) cases. Among the benign cases, halo sign present in 34 (79.1%) cases and absent in 7 (20.9%) cases. Among the malignant cases, halo sign present in 1 (9.1%) cases and absent in 10 (90.9%) cases.
Out of all cases 15 were diagnosed as having malignant nodule by USG and among them 10 were confirmed by histopathological evaluation. They were true positive. Five cases were diagnosed by as having malignant nodule by USG but not confirmed by histopathological findings. They were false positive. Of 37 cases which were confirmed by USG as benign, among them 1 was confirmed as having malignant nodule and 36 were confirmed benign by histopathological. They were false negative and true negative respectively. Nggada et al. (2006) I a showed that 73.9% cases were benign and 26.1% were malignant. Their study findings comparable with present study. Binesh and Salari, (2008) in a study of 600 cases (91 male. 509 female) the cytological diagnosis was as follows: 87.7% benign, 4.7% malignant, 1.6% suspicious and 6% unsatisfactory. Between benign lesions, goiter and follicular adenoma and between malignant lesions, papillary cell carcinomas were the most common.
Sensitivity of USG to diagnose malignant thyroid nodule was 90.9%, specificity 87.8%, positive predictive value 66.7%, negative predictive value 97.3% and accuracy 88.5%. In a study Stacul et al (2007) correlated the diagnosis of benign or malignant thyroid nodules obtained with grey-scale ultrasound (US) and color- Doppler US with the cytological findings. Their result was not comparable with our series. The sensitivity, specificity, PPV, NPV and overall accuracy values of grey-scale US of their series were 46%, 73%, 34%, 82% and 67%, respectively for solitary thyroid nodules and 35%, 72%, 14%, 90% and 68% respectively for multiple nodules.
SUMMARY
Total 52 patients with thyroid pathology were included in the present study. The Summary of the present study as followed:
Among the 11 (100%) malignant cases all were found in single thyroid nodule. None found in multiple thyroid nodules. The 7 were multiple nodules and all were benign cases
Out of all patient having benign nodules 85.4% had regular and 14.6% had irregular margin. In malignant nodule all had irregular margin.
Among the benign cases 41.5% were solid, 4.9% were cystic, 39.0% were complex mass and 14.6% were solid with solid cystic change. No benign case was found hypoechoic. Among all malignant cases 18.2% were solid, 45.5% were complex mass and 36.4% were hypoechoic. All hypoechoic lesions were malignant. All cystic and solid with cystic lesion were benign.
Among the 52 respondents, calcification present in 32 (59.3%) case and absent in 20 (40.7%) cases in ultrasonographic findings.
Out of all cases 15 were diagnosed as having malignant nodule by USG and among them 10 were confirmed by histopathological evaluation. They were true positive. Five cases were diagnosed s having malignant nodule by USG but not confirmed histopathological findings. They were false positive. Of 37 cases which were confirmed by USG as benign, among them 1 was confirmed as having malignant nodule and 36 were confirmed benign by histopathology. They were false negative and true negative respectively.
Sensitivity of USG to diagnose malignant thyroid nodule was 90.9%, specificity 87.8%, positive value 66.7%, negative predictive value 97.3% and accuracy 88.5%.
CONCLUSION
This cross section study was carried out in the department of Radiology and Imaging, DhakaMedicalCollegeHospital, Dhaka with an aim to determine the usefulness of ultrasonography in the detection thyroid nodular pathology and its correlation and / or histopathological findings. There are certain characteristics of thyroid nodules seen on ultrasound and the ultrasound alone cannot make the diagnosis of cancer. The result of the current study showed that the correlation between the ultrasonographic findings and histopathology of the thyroid nodule is a highly reliable tool with which assessment of a nodule is benign or malignant and to plan the subsequent appropriate therapy in the vast majority of cases.