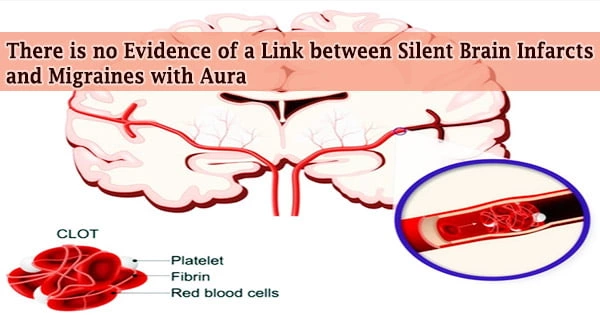
A large cross-sectional study compared the brain MRI images of women with migraines with aura to those of women who did not have migraines. There were no variations in the number of silent infarcts or white matter hyperintensities (WMH) between these two groups of women. The research was published in the journal Brain.
A migraine is a severe headache that is often accompanied by nausea, vomiting, and light sensitivity. It could linger for hours or even days. Migraine is a frequent health problem that affects one out of every five women and one out of every fifteen males. They usually start while a person is in their early twenties.
Migraines affect more than a tenth of the female population. One out of every three of these patients has migraines with aura, which are characterized by transient neurological symptoms that occur in conjunction with migraine attacks.
Migraine headaches are a symptom of migraine disorder. Doctors aren’t sure what causes migraine headaches, although they appear to be linked to changes in the brain and DNA.
Previous research has highlighted concerns about a possible link between migraines and an elevated risk of silent brain infarcts and white matter hyperintensities, particularly in migraine sufferers who have an aura. WMHs and silent brain infarcts have been linked to an increased risk of dementia.
Infarcts identified by neuroimaging or necropsy without a history of stroke are known as silent brain infarcts. Ischemic symptoms may have gone unnoticed or forgotten by the patient, or they may have been just temporary.
“This prompted us to evaluate whether women with migraine with aura might be more likely to have evidence of silent brain infarcts and an increased load of white matter hyperintensities on their brain scans,” says research team leader Dr. David Gaist of the Odense University Hospital and the University of Southern Denmark.
This prompted us to evaluate whether women with migraine with aura might be more likely to have evidence of silent brain infarcts and an increased load of white matter hyperintensities on their brain scans.
Dr. David Gaist
Infarcts that are silent are prevalent. On computed tomography (CT), infarcts are observed in roughly 15% of patients with asymptomatic carotid artery lesions. Furthermore, examining the processes of SBI directly is difficult due to the fact that these lesions are nearly typically discovered by chance and are of unknown age.
The small size of many SBI, their inconspicuous placement, and chronic ischemia preconditioning are all appealing explanations for why certain cerebrovascular incidents do not appear clinically.
The Danish Twin Registry helped the researchers find women between the ages of 30 and 60. They were able to identify 172 women with migraine with aura (cases) and 139 unrelated women without migraine (controls) who had MRI brain imaging at a single center thanks to this nationwide registry.
Migraines have no established cause, but they’re assumed to be caused by transitory alterations in the brain’s chemicals, neurons, and blood vessels. Around half of all migraine sufferers also have a close relative who suffers from the disease, implying that heredity may play a role.
Thirty-four co-twins who did not suffer from migraine with aura, unlike their participating twin sisters, were also scanned.
“We found no evidence of an association between migraine with aura and silent brain infarcts or white matter hyperintensities,” says Dr. Gaist.
“This held true for the main analyses comparing cases with unrelated controls, and for analyses focusing on twin pairs where one twin suffered from migraine with aura, and the other did not.”
“We believe patients suffering from migraines with aura and their physicians should find these results re-assuring,” says Dr. Gaist.