Symptoms are frequently the result of the body’s response to an infection or illness. They can serve as warning signs that something is wrong, assisting the individual and healthcare professionals in identifying and treating the underlying problem. Symptoms vary according to the disease and the individual’s immune response.
Scientists discovered that combining specific diets with diarrheal disease-causing bacteria can create long-lasting immunity in mice without the need for symptoms. The findings pave the way for the development of vaccines that could reduce the symptoms and mortality associated with diarrheal illness and other diseases in humans.
Every year, more than a million people die as a result of diarrheal diseases, which cause dehydration and malnutrition. However, no vaccine exists to combat or prevent these diseases caused by bacteria such as certain strains of E. coli. Instead, people with bacterial infections must rely on their bodies to employ one of two defence strategies: kill the intruders or impair the intruders while keeping them alive. If the body chooses to impair the bacteria, the disease can occur without diarrhoea, but the infection can still be transmitted – this is known as asymptomatic carriage.
Salk scientists have discovered that combining specific diets with disease-causing bacteria can create long-lasting immunity in mice without incurring the costs of illness, revealing a new potential vaccination strategy. Their findings, which will be published in Science Advances on June 23, 2023, pave the way for the development of new vaccines that could boost immunity in people suffering from diarrheal diseases and possibly other infections.
We discovered that immunization against diarrheal infections is possible if we allow the bacteria to retain some of its disease-causing behavior. This insight could lead to the development of vaccines that could reduce symptoms and mortality, as well as protect against future infections.
Professor Janelle Ayres
“We discovered that immunization against diarrheal infections is possible if we allow the bacteria to retain some of its disease-causing behavior,” says senior author Professor Janelle Ayres, Salk Institute Legacy Chair and head of the Molecular and Systems Physiology Laboratory. “This insight could lead to the development of vaccines that could reduce symptoms and mortality, as well as protect against future infections.”
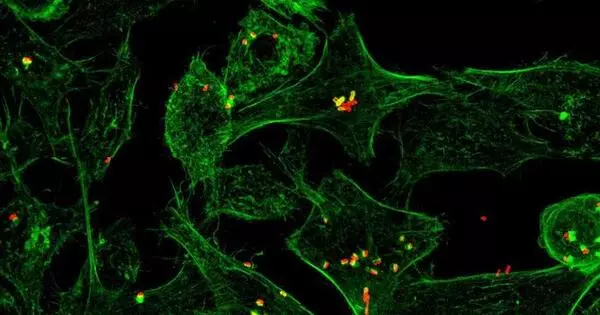
In 2018, Ayres’ lab investigated how dietary interventions can induce an asymptomatic infection, which Ayres defines as a cooperative relationship between bacteria and host (the person or animal infected by the bacteria) in which the host does not exhibit any symptoms. They discovered that an iron-rich diet allowed mice to survive a normally fatal bacterial infection without showing any signs of illness or disease. The high-iron diet increased unabsorbed sugar (glucose) in the mice’s intestines, providing food for the bacteria. The extra sugar acted as a “bribe” for the bacteria, keeping them satiated and incentivized not to attack the host.
This process produced long-term asymptomatic infection with the bacteria, leading the researchers to believe that the adaptive immune system (cells and proteins that “remember” infections) may be involved.
“Using established vaccination strategies, it has not been possible to generate long-lasting immunity against bacteria such as C. rodentium or E. coli. We wanted to figure out what mechanism was sustaining this lasting immunity so we could use that mechanism to create an impactful solution to these diarrheal diseases,” says Grischa Chen, first author and former postdoctoral researcher in Ayres’ lab.
The researchers set out to discover how the body suppresses infection symptoms, whether infection without symptoms can result in long-term immunity, and whether that immunity can be replicated as a vaccination strategy.
The team compared mice with iron-rich and normal diets after C. rodentium infection to find whether the diet impacted symptomless infection. Immediately after infection, mice fed an iron-rich diet had no symptoms whereas mice fed a normal diet did have symptoms. All mice were then put on a normal diet to see whether the asymptomatic infection would last.
Mice with nonfunctional adaptive immune systems (the immune system that “remembers” previous infections) could not maintain a cooperative relationship with the bacteria, regardless of whether they had ever been on an iron-rich diet. Although an iron-rich diet alleviated symptoms immediately following infection, the adaptive immune system was required for long-term cooperation. Importantly, mice with functional adaptive immune systems survived the disease with no symptoms and long-lasting immunity, as evidenced by survival after reinfection after a month.
Ayres and colleagues came to the conclusion that an iron-rich diet alone can prevent bacteria from causing lethal symptoms in mice during active infection. In the absence of dietary supplementation, a functional adaptive immune system is required for immunity against future infection.
Some bacterial strains, when sufficiently mutated, do not cause symptoms. To see if such bacteria could induce long-term immunity, the researchers repeated their iron-diet versus normal-diet experiment in mice, but this time with bacteria that could cause disease and bacteria that could not. They discovered that only mice given disease-causing, unmutated bacteria could support immunity during reinfection.