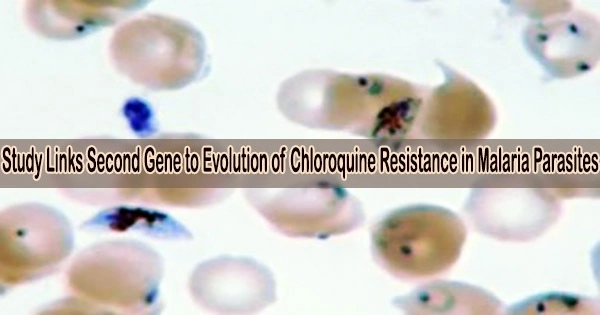
It has long been assumed that just one crucial gene played a role in how malaria parasites evolved to resist a potent antimalarial medication. An international research team has now demonstrated that a second crucial gene is also involved in malaria’s resistance to the medication chloroquine as a result of a combination of field and lab experiments.
The discovery, which was made this week and was published in the journal Nature Microbiology, has repercussions for the ongoing fight against malaria, which is thought to affect 247 million people worldwide and kills more than 619,000 people yearly, largely young children.
“With drug-resistant pathogens on the rise, it is important to understand how treatments drive parasite evolution and how this evolution can vary in different parts of the world,” says Texas Biomedical Research Institute Professor Timothy J.C. Anderson, Ph.D., one of the lead authors of the paper.
Chloroquine was developed to treat malaria in the 1950s and administered widely. Within a short period of time, drug resistance developed and expanded, first through Southeast Asia and then through Africa in the 1970s and 1980s. Chloroquine was eventually replaced by a series of other antimalarial medications, however controlling the parasites is still difficult due to resistance evolution.
In order to assist the parasites move chloroquine out of a crucial area of their cells and render the medication useless, the gene known as the chloroquine resistance transporter (pfcrt) evolved, according to a study published in 2000.
“That resistance gene, pfcrt, is infamous,” says University of Notre Dame Professor Michael Ferdig, Ph.D., and one of the lead paper authors. “To find that pfcrt has a partner in crime should not be a surprise genes interact with each other as part of evolution all the time. But it was only with new tools and our integrated approach that we could finally pinpoint the specific culprit.”
Our analyses showed that parasites from Africa and Asia carry different pfaat1 mutations, and our experimental data suggest that this may underlie the differences we observe in drug resistance evolution in Africa and Asia.
Professor Michael Ferdig
Six species of malaria parasites infect humans; Plasmodium falciparum is considered the deadliest. In this paper, researchers from the Medical Research Council Unit The Gambia at the London School of Hygiene & Tropical Medicine and collaborators analyzed more than 600 P. falciparum genomes collected in The Gambia from 1984 to 2014.
The 30-year dataset revealed that mutations in a second gene encoding an amino acid transporter (AAT1) increased from 0% frequency in 1984 to 97% frequency in 2014.
“This is a very clear example of natural selection in action these mutations were preferred and passed on with extremely high frequency in a very short amount of time, suggesting they provide a significant survival advantage,” says Medical Research Council Unit The Gambia at London School of Hygiene & Tropical Medicine Professor Alfred Amambua-Ngwa, Ph.D., and one of the first authors. “The mutations in AAT1 very closely mirror the increase of pfcrt mutations. Given this, it strongly suggests AAT1 is involved in chloroquine resistance.”
To assess experimentally how the mutations affect treatment resistance, teams from Texas Biomed, University of Notre Dame, and Seattle Children’s Research Institute worked together. AAT1 mutations may be involved, according to research on genetic crosses between chloroquine-sensitive and chloroquine-resistant parasites.
Researchers altered the mutations in the parasite genomes in the lab using CRISPR gene-editing technology, and they noticed how this affected medication resistance. Researchers from Nottingham University examined the gene’s activity in yeast, and the results revealed that the mutations led to drug resistance. Collaborating institutes also included Wellcome Sanger Institute, Mahidol-Oxford Tropical Medicine Research Unit and UT Health San Antonio.
“This project would not have been possible without the dedication of multiple collaborators in the US, Europe, Asia and Africa,” says Ashley Vaughan, Ph.D., principal investigator at Seattle Children’s Research Institute, and one of the lead paper authors. “We brought together very diverse methodologies, which all came to the same conclusion.”
But the team did not stop there. Additional malaria genome datasets revealed that, as would be predicted, the AAT1 mutations that confer resistance vanished in Africa once chloroquine use was discontinued. Southeast Asia, where the mutations persist, is a very different picture.
“Our analyses showed that parasites from Africa and Asia carry different pfaat1 mutations, and our experimental data suggest that this may underlie the differences we observe in drug resistance evolution in Africa and Asia,” says Dr. Ferdig.
Surprisingly, more than ten years ago, researchers investigating various malaria species that affect rats discovered the same gene to be implicated in chloroquine resistance.
“This shows me that the rodent and human malaria researchers need to be talking more,” Dr. Anderson says.
Professor David Conway, Ph.D., of the London School of Hygiene & Tropical Medicine emphasizes the need for a comprehensive strategy to both drug research and pathogen surveillance in order to combat medication resistance for malaria and other diseases.
“We must be aware that different genes and molecules will be working together to survive treatments,” he says. “That’s why looking at whole genomes and whole populations is so critical.”