Background Child malnutrition is one of the most serious public health problems in the developing world includingBangladesh. In the 1950s, the United Nations and its agencies became involved in evaluating the extent of the problem, and malnutrition (M) became the subject of worldwide study. Since then, considerable resources have been directed towards improving treatment of those suffering from this serious and complicating conditions; despite this, for those who received treatment, reported care fatality rates range from 4.4% to 4.9%, with even higher rates for edematous cases. The World Health Organization (WHO) defines malnutrition as “the cellular imbalance between the supply of nutrients and energy and the body’s demand for them to ensure growth, maintenance, and specific functions.” The term malnutrition refers to both under nutrition as well as over nutrition. However, in maximum cases, the terms malnutrition and PEM are used interchangeably with under nutrition. The term protein-energy malnutrition (PEM) applies to a group of related disorders that include marasmus, kwashiorkor, and intermediate states of marasmus-kwashiorkar.2Three anthropoemetric indicators are commonlyused to describe the nutritional status of the children: weight-for-height(wasting), height-for-age(stunting) and weight-for-age(underweight). A deficit in any of these reflects malnutrition and a Z-score below -3 indicates severe form of illness. Malnutrition limits the potential of a country and is strongly associated with mortality, morbidity, reduced cognitive performance and compromised productivity among its population. Malnutrition and infection interact in a vicious cycle. The presence of one or more easily leads to the development of the other and they have a biological synergism that causes the effects of either to be increased in the presence of the other. Healthy child growth and development is the basis of human development. The impact of malnutrition is multifarious. It has an all-pervasive impact on the physical well-being and socioeconomic condition of a nation. It perpetuates poverty through direct losses in productivity, indirectly losses from poor cognitive function, poor child development and deficits in schooling and losses due to increased health costs. Malnutrition due to deficiencies and to excesses is strongly correlated with social and economic inequalities. Chronic protein-energy malnutrition may lead to stunting, defects in mental and physical performance, and decreased resistance to infectious disease. Childhood malnutrition has serious consequences that make prevention and control imperative.5PEM is more of a social problem i.e., the biological translation of a social disease. PEM’s basic causes stem from inadequate resources, poor resource utilization and lack of control of resource. The compounding effects of both underlying and immediate causes are eventually responsible for its manifestation. Malnutrition remains one of the most common causes of morbidity and mortality among children throughout the World.It has been responsible, directly or indirectly, for 60% of the 10.9 million deaths annually among children. Well over two third of these deaths, which are often associated with inappropriate feeding practices, occur during the first year of life. According to the State Of the World’s Children (SOWC) report 2008, issued by the UNICEF, eight million or 48 percent of all children under five are underweight malnutrition contributes to about that of all Child deaths.10One out of four children, roughly 146 million in developing countries are underweight. 10.9 million children under- 5 die in developing countries each year. More than 70% of the World’s 146 million under age 5 years live in just 10 countries and more than 50% located in South Asia alone. Although, there is a perception that the situation of malnutrition among children is worst in Africa, the problem of malnutrition is much higher in South Asia, for instance, the prevalence of underweight among preschool children is almost double in Bangladesh compared to Somalia or Mozambique and equal to that of Ethiopia. The scenario of Bangladesh is much frightening as it poses a major bulk of the malnourished children of the developing countries through the situation is slowly improving here from nineties.14Bangladesh is one of the three countries in South Asia region that accounts for half the world’s malnourished children (United nations children’s fund 2006).In Bangladesh, 1.2% of the 17 millionunder-five children, approximately 200,000 believed to be severely wasted. But according to new WHO Growth reference Standard 2006, the proportion of children with severe wasting is 2.9% thus the total number being 500,000. Problem Statement Malnutrition is widespread in most developing countries and it is particularly prevalent among the children as they are the most vulnerable group of a society. The problem is more serious in Bangladesh where poverty and illiteracy are predominating.This is implication of the fact that, we are heading towards a nation that will see its children to be of small poor status and low intellectual population. So we need to give the highest priority to child health and nutrition if we hope for a brighter future of our country. According to BDHS 2011 the prevalence of malnutrition in under five children are as follows:41% children are stunted, 15% are severely stunted, 17% children are wasted and 4% are severely wasted, 36% children are underweight and 10% are severely underweight. According to the criteria of WHO (WHO,1995), the children also have high rates of diarrheal infections, nutritional blindness, morbidity and mortality. These high rate of malnutrition may be attributed to poor environmental sanitation, overcrowding, lack of preventive and curative health services and others socio-economic, cultural and educational factors.Feeding practices have long been recognized as potentially important determinants of child malnutrition. Although the breast feeding rate in Bangladesh is satisfactory, the high rate of child’s severe malnutrition signifies the operation of other important factorssuch as inadequate supplementation and delayed weaning etc. As malnutrition is a man-made disease of human society, socio-economic status of a family plays also an important predisposing factor regarding SAM. Therefore, a first step to understand malnutrition and child health in a particular community is to have a thorough knowledge of the status of malnutrition and factors associated with the child feeding of that community. Nutritional status is the best global indicator of well-being in children. Child malnutrition is also an important indicator of monitoring progress towards the millennium development goals (MDGs). The death rate among children hospitalized for severe acute malnutrition was as high as 15 percent.18 So SAM contributes a major role in under five mortality rate in Bangladesh. If we can lessen it,then it is possible for us to achieve the Millennium Development Goal target for under five mortality rate to 48/1000 live births more rapidly and also declining malnutrition prevalence to 34%by 2015. Literature Review Niger T M et al. studied among two hundred and twenty five mothers of Dhaka medical college hospital are interviewed to investigate of determinants of malnutrition. All of our respondents were under two years of age. One hundred fourteen of them were girls and rests 111 were boys. All of the children were from different socio-economic status coming different places of Bangladesh. 28% of the respondents’ family monthly incomes were below 3001-5000, 3.6% were below 20,000-25,000 and 16.4% were 10,000-15,000, 21.3% respondents’ mothers were illiterate, 24.4% mothers were primary level, 32% mothers were secondary level, 11.1% mothers were higher secondary level and 11.1% were graduate. The nutritional status children were not found very from normal to 3rd degree malnourishment. Nearly 45.8% were normal, 1.8% was over nourished and 2.2% were 3rd degree malnourished. In the above context, it can be concluded that a large number of the population of Bangladeshi children are suffering from malnutrition (more than half) and are likely to grow smaller and smaller. This is implication of the fact that we are heading towards a nation that will see its children to be of small status and low weight population. So, we need to give highest priority to child health and nutrition if we hope for a brighter future of our country. Iqbal H M et al. conducted a study about nutritional and immunization status, weaning practices and socio-economic conditions of under five children in three villages of Bangladesh. They showed in their study that, low household income, parental illiteracy, small family size (< or = 6), early or late weaning and absence of BCG vaccination were significantly associated with severe PEM. Timely weaning, education and promotion of essential vaccination may reduce childhood malnutrition especially severe PEM. Nahar B et al.(2010) have conducted a case control study in Dhaka hospital of ICDDR,B and found in their study that, severely-underweight children were more likely to have: undernourished mothers mass index (BMI)<18.5, who wereaged <19 years and completed <5 years of educationhad a history of shorter duration of predominant breastfeeding (<4 months), discontinuedbreastfeeding , had higher birth-order >3, fathers who were rickshaw-pullers or unskilled day-laborers and completed<5 years of education, came from poorer families monthly income of Taka <5,000,Parental education, economic and nutritional characteristics, child-feedingpractices, and birth-order were important risk factors for severe underweight in this population, andthese characteristics can be used for designing and targeting preventive intervention programs. M. OWOR et al.(2000) conducted a case control study in Mulago Referral and Teaching Hospital, Kampala, Uganda to determine socio-economic risk factors for severe PEM among children. They took sixty six severely malnourished children (age 0-60 months) were matched, for age and sex, with 66 well-nourished controls, and socio-economic, demographic, health facility utilization and feeding practices were compared between the two groups. Severe protein energy malnutrition was associated with young age of the caretaker, living in a mud walled house, lack of breast feeding, failure to complete immunization, no land ownership, and no ownership of livestock, by the caretaker. The level of formal education of the caretaker was not associated with severe malnutrition. Rahman A and Biswas S Cused data from the 1999-2000 Bangladesh Demographic and Health Survey (BDHS) in their study toexplore nutritional status of children aged 0-59 months. The prevalence of malnutrition is assessed by three standard anthropometric indicators: underweight, stunting and wasting, following the WHO guidelines and cut-off points. The distributions of Z-scores for the study children showed considerably far downward distributions for all indicators from the reference population mean zero. In addition, total stunting, wasting and underweight were observed in 44%, 10% and 47% (among them 18%, 1% and 13% were severely stunted, wasted and underweight) of the children respectively and the trends in prevalence of malnutrition are increasing after the 1999-2000 BDHS. The study points out that, malnutrition is one of the most critical components for child health that affects almost 56.5% Bangladeshi children. Reassessment of current policies and further appropriate interventions should be formulated to improve socioeconomic and maternal conditions to reduce the overall burden of malnutrition. Mitra M et al. conducted a study to assess child malnutrition and delineate the factors contributing to the observed pattern of malnutrition among preschool children from three specific population namely-Saryupari Brahmin, Teli and Rawat of Raipur district of Chattisgarh, India through nutritional anthropometric survey. The nutritional anthropometric data collected on 121 Saryupari Brahmin (57 boys and 64 girls), 93 Rawat (49 boys and 46 girls) and 97 Teli (46 boys and 51 girls) children ranging in age from 2+ to 5+ years. The pattern of protein- energy malnutrition observed is primarily of mild to moderate intensity in Brahmin and moderate to severe intensity in Rawat and Teli children. The findings clearly indicate towards various socio economic and micro-environmental factors as probable contributors towards poor nutritional status. All these observation suggest that preschool children need better nutrition and health care combat the problem of PEM. Ahmed A E et al.conducted a study to identify the risk factors of protein energy malnutrition among children underfive years of age in Assiut university children hospital, Egypt. A correlation descriptive research design was chosen for thisstudy. A convenient sampling design was followed to include children suffering from protein energy malnutrition aged below 5 years. Control group was purposively selected to be nearly age and sex matched. The results revealed that PEM was more found in children in families of middle and low socioeconomic status with statistically significant differences, history of malnutrition in other sibling and younger age than others, statistically significant differences between practices of mothers in the cases than thecontrol groups were found regarding breast feeding, artificial feeding and additional and adult food with low level ofsatisfactory practices observed among mothers in the cases than those in the control groups. From this study it can be concluded that several risk factors were found to be associated with PEM including, lower education level of the mother, number of children in the family as the number of children in the family decreased , the prevalence of PEM increased, low and middle family socioeconomic status, age of the child, children with the younger age are more vulnerable to have PEM than those of older age and mothers’ practices regarding feeding of their children (breast feeding, artificial feeding as well as additional and adult food) unsatisfactory practices of mothers regarding feeding of their children increase the prevalence of PEM among their children. This study recommended that Supporting and promotion of breast feeding, avoid using of artificial feeding and bottles, health education to the mothers about proper feeding practices, breast feeding, artificial feeding and additional and adult food to prevent PEM, increasing mother’s awareness related to risk factors of PEM and how to manage the different infections among their childrenand encourage vaccination at the appropriate time. Singh A K et al. conducted A cross-sectional study by house to house visit covering 406 children (1-6 years) from the sub center villages of Meerut district in India to see the socio-economic status. They showed that the prevalence of underweight was 57.4% according to IAP classification with the proportion of grade I, II and III under nutrition being 68.2%, 29.2% and 2.6% and none of the children in grade IV under nutrition. The prevalence of underweight was significantly higher in 3-6 years children (64.1%) as compared to 1-3 years children (47.6%) and there was no significant difference in the sex and caste. Prevalence of underweight was significantly higher in children belonging to nuclear families. There was direct association of underweight in relation to poor housing and environmental sanitations and low standard of living index. The prevalence of underweight was low in children of literate mother. Ayaya S O et al.pointedrisk factors for severe protein energy malnutrition (PEM)as ignorance, family size, mothers and fathers education, poverty, residence, chronic infections, and congenital defects or malformations. The role of such social factors as the caretaker, extended family, homestead surroundings, and family cohesiveness has not been studied in Kenya.To determine the social and economic factors that predispose children to severe PEM as seen at the Moi Teaching and Referral Hospital (MTRH), Eldoret they conducted a Prospective and case control study .Here sixty six children aged 3 to 36 months with severe PEM attending the MTRH outpatient clinics and those admitted in the Pediatric wards were age-matched with 66 controls.The social risk factors for PEM were single mothers,young mothers aged, the child’s living conditions such as living in a temporary house, caretaker who was not married to the child’s parentand not staying with both parents in the past six months.The economic risk factors were father’s lack of ownership of land, cattle not growing maize, not growing beans and ownership of small piece of land by grandfather. Other risk factors were incomplete immunization and female sex. R O et alstated that, three hundred and seventy pre-school children (181 males and 189 females) were studied in order to document the prevalence of protein energy malnutrition and factors that militate it. The prevalence of protein energy malnutrition among the children was revealed to be 41.6%(154). One hundred and fifty-one (40.8%) of them were found to have weight-for-height below -2SD indicating level of stunting among the children. Most malnourished children belonged to mothers who were illiterate 97 (54.8%) when viewed from the mothers’ educational perspective. This study also showed the following factors that were statistically significant with PEM: educational status of mothers (p<0.05), marital status (p<0.05) of mothers, occupational status of mothers (p=0.000), parental income per annum (p=0.000), length of breastfeeding (p=0.000), water supply and regularity, type of housing and toilet facilities. Justification of the Study Children who have severe malnutrition, particularly with onset at an early stage, do not achieve their growth potential or regain cognitive deficits. Moreover, mortality remains very high in SAM and the children who are admitted to hospital with malnutrition represent only the tip of the iceberg. Despite the manifold dietary approaches to severe malnutrition that have been tried, patients continue to die much more frequently.Studies showed that malnutrition is the worst in Bangladesh, for instance, the prevalence of child malnutrition in Bangladesh is among the highest in the World.30 As long as severe malnutrition is prevalent in this country, efforts to improve its knowledge, treatment and outcome are a priority. In Bangladesh, several studies regarding malnutrition have been carried out, mostly in rural areas. In urban areas, such type of study has been found scant specially in dense overcrowded city like Dhaka. According to BDHS 2011, the prevalence of severely wasted child (4.3%) is more than any other city even from rural areas. This study will be of much importance to unveil the causes and magnitude of existing SAM in a tertiary hospital for overall prevention and treatment of severe protein-energy malnutrition in other facility based management centers. Operational Definitions
- Nutrition
It is the science of food, the nutrients and other substances within food, their actions and interactions and balance in relation to health and disease.
- Malnutrition
Malnutrition includes a wide range of clinical disorders resulting from an unbalanced intake of energy, protein as well other nutrients. It can present as under or over nutrition.
- Protein-Energy-Malnutrition (PEM)
Protein-Energy-Malnutrition is a clinical syndrome present in infants and children as a result of deficient intake and/or utilization of food.
- Severe Acute Malnutrition (SAM)
A child aged 6 to 59 months is classified as severely malnourished8 if s/he has one or more of the following: (1) Weight- for- Height Z-score (WHZ) <-3 (2)Mid-upper arm circumference (MUAC) <115 mm (3) Bipedal edema
- Weight-for-Height; reflects body mass relative to height;
A child below minus two standard deviation (-2SD) from the reference median for the weight-for-height is considered to be too thin for his / her height, or wasted, a condition reflecting acute or recent nutritional deficiency. If the child is below -3SD, wasting is considered severe. It is closely link to mortalityrisk.
- Weight-for-Age; reflects body mass relative to chronological age;
It is composite index of weight-for-height and height-for-age and this does not distinguish between acute malnutrition (wasting) and chronic (malnutrition stunting)
- Height-for-Age; reflects height relative to chronological age;
Height-for-age is a measure of linear growth. A child who is below -2SD. From the median of the WHO reference population in term of height-for-age is consider stunted, a condition reflecting the effect of chronic malnutrition. 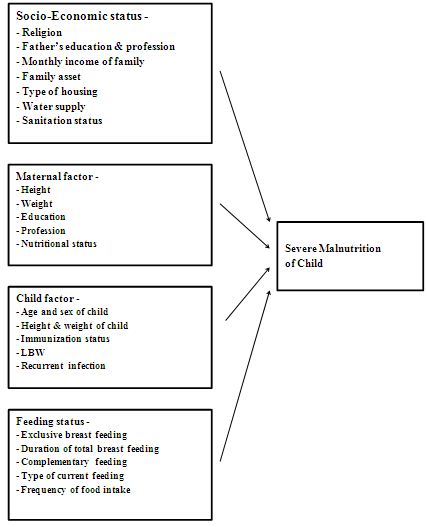 4. Research question What are the nutritional statusand determinants of Severe Acute Malnutrition among under 5 years old children in a tertiary care hospital of Dhaka ? Objectives General objective To assess the nutritional statusand determinants on Severe Acute Malnutrition among under 5years old children in a tertiary care hospital of Dhaka. Specific objectives
4. Research question What are the nutritional statusand determinants of Severe Acute Malnutrition among under 5 years old children in a tertiary care hospital of Dhaka ? Objectives General objective To assess the nutritional statusand determinants on Severe Acute Malnutrition among under 5years old children in a tertiary care hospital of Dhaka. Specific objectives
- To assess the nutritional statusof SAM among enrolled children.
- To determine the socio-economic factors of the SAM children.
- To find out the maternal and child factors affecting the SAM children.
- To identify the feeding factors ofSAMamong enrolled children.
Methodology Study area Dhaka Shishu Hospital, Dhaka Study period and duration April – July 2013 Study population Under 5 years old children in Dhaka Shishu Hospital, Dhaka. Study design Descriptive Cross sectional study Sample Technique Under 5 years old children who will be admitted in Dhaka Shishu Hospital during the study period will be consecutively enrolled in the study after consideration of inclusion and exclusion criteria from register record by using purposivesampling technique. Selection of samples (a)Inclusion Criteria:
- Age: Less than 5 years old children
- Sex: Irrespective of sex.
- WHO criteria of severe malnutrition if the child has one or more of the following –
→ Mid-upper arm circumference <115mm. → Weight-for- height Z-score (WHZ) <-3 → Bipedal edema. (b) Exclusion Criteria:
- Children less than 6 months of age.
- Patient with secondary malnutrition due to other causes like DiabetesMellitus, Hyperthyroidism, Congenital Anomalies, Cerebral Palsy, HeartDisease, Kidney Disease etc.
- Patient with edema due to Congestive Heart Failure, Cirrhosis of Liver,Protein Losing Enteropathy.
- Children with their parents coming from outside Dhaka division.
Data collection Method Children will be enrolled from admitted patients during the period between April 2013 to July 2013. A structured investigation administer questionnaire (proforma) will be used to obtain information from the children’s mother. For each child, a detailed history, age, sex, nutritional status, birth history, immunization status, socio-demographic, maternal education, economic history like family income of parents will be recorded and anthropometric measurements will be done subsequently. Facilities available at the place of study: Dhaka Shishu Hospital is a 600 bed tertiary care hospital in Bangladesh providing care of children for all over Bangladesh. All equipment is readily available to collect data. Infantometer, stadiometer and flexible, plastic measuring tape with a width of 1 cm and subdivision of 0.1 cm will be used to measure length or height of a child and mother. Baby scale, Bathroom scale or digital weight machine (DETECTO MB 130, 10/20 kg d=5/10 gm) will be used for weight measurements of child and mother. Data management and analysis Collected data were checked, verified and compiled to maintain validity of contents of data. The Anthro 2005 software of WHO will be used for calculating Z-score. SPSS version 17 will be used for analysis where p value less than 0.05 will be taken as a significant value. Descriptive statistics along with necessary statistical interpretations will be made with the data Ethical issues Informed written consent will be taken for this study. Procedure will be discussedwith the guardian. Confidentiality will be maintained and participants can withdraw their names any time from the study Clearance will be taken from the ethical review committee of Dhaka Shishu (Children) Hospital. 















