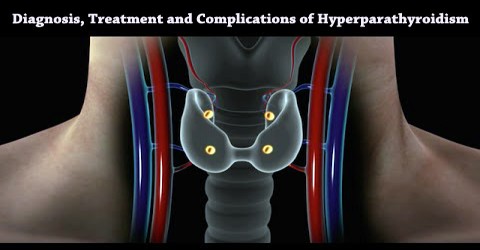
Diagnosis, Treatment and Complications of Hyperparathyroidism
Introduction
Hyperparathyroidism is the presence of excess parathyroid hormone in the body resulting in disturbance of calcium metabolism with increase in serum calcium and decrease in inorganic phosphorus, loss of calcium from bone, and renal damage with frequent kidney-stone formation.
Primary hyperparathyroidism is a disorder of the parathyroid glands in which one or more of the parathyroid glands are enlarged (hyperplastic), overactive, and secrete too much parathyroid hormone. In secondary hyperparathyroidism, the parathyroid glands themselves are normal but a problem such as kidney failure makes the body resistant to the action of parathyroid hormone.
Diagonsis of Hyperparathyroidism
Hyperparathyroidism is usually diagnosed after blood tests have shown a high level of calcium and a high level of parathyroid hormone. Usually, the level of phosphate in our blood is low. Tertiary hyperparathyroidism has a high PTH and high serum calcium. It is differentiated from primary hyperparathyroidism by a history of chronic kidney failure and secondary hyperparathyroidism.
Blood Tests: Additional blood tests can help our primary care provider make a more accurate diagnosis. Our primary care provider will check our blood for high PTH levels, high alkaline phosphatase levels, and low levels of phosphorus.
Urine Tests: A 24-hour collection of urine can provide information on how well our kidneys function and how much calcium is excreted in our urine. This test may help in judging the severity of hyperparathyroidism or diagnosing a kidney disorder causing hyperparathyroidism. If a very low level of calcium in the urine is found, this may indicate a condition that doesn’t require treatment.
Kidney Tests: Our primary care provider might take X-rays of our abdomen to check for kidney abnormalities.
Bone Mineral Density Test (bone densitometry): The most common test to measure bone mineral density is dual energy X-ray absorptiometry, or a DXA scan. This test uses special X-ray devices to measure how many grams of calcium and other bone minerals are packed into a segment of bone.
Ultrasound: Ultrasound uses sound waves to create images of our parathyroid glands and surrounding tissue.
Treatment of Hyperparathyroidism
Surgery to remove the enlarged gland(s) is the only treatment for hyperparathyroidism (HPT) and cures 95 percent of cases. The growth typically does not return and symptoms disappear after the first month of surgery. For a short time after surgery, our blood calcium level may be too low, which is easily treated with medicine. If surgery is not recommended because of other medical conditions, medicines are available to treat some of the symptoms of HPT. Some patients who have a mild form of the disease, are symptom-free, only have slightly elevated blood calcium levels and whose kidneys and bones are normal may not need surgery. In these cases, patients require monitoring of their calcium and kidney functions ever six months as well as abdominal X-rays and bone mass measurements after one to two years.
Hormone replacement therapy can help bones hold on to calcium. This therapy can treat postmenopausal women with osteoporosis, although there are risks involved with prolonged use. These include an increased risk of some cancers and cardiovascular disease.
People with primary hyperparathyroidism who are symptomatic benefit from surgery to remove the parathyroid tumor (parathyroid adenoma). In people with secondary hyperparathyroidism, the high PTH levels are an appropriate response to low calcium and treatment must be directed at the underlying cause of this, usually vitamin D deficiency or chronic kidney failure. If this is successful PTH levels should naturally return to normal levels unless PTH secretion has become autonomous (tertiary hyperparathyroidism). The ideal situation is that tertiary hyperparathyroidism does not develop because secondary hyperparathyroidism is successfully treated. However, if it does develop, the treatment of tertiary hyperparathyroidism is usually surgery to remove the overactive parathyroid glands.
Complications of Hyperparathyroidism
Not everyone with hyperparathyroidism has complications. However, sometimes complications may develop. If anyone have primary or tertiary hyperparathyroidism, these complications are mostly due to a long-standing high level of calcium in their blood.
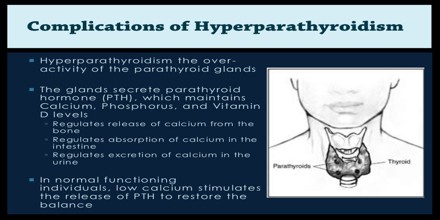
If people suffer from hyperparathyroidism, they might also have a condition called osteoporosis which is also sometimes referred to as “thinning” of the bone. Common symptoms include bone fractures and height loss due to vertebral body (spinal column) fractures. This can develop when excess PTH production causes too much calcium loss in your bones, making them weak. Osteoporosis typically occurs when people have too much calcium in their blood and not enough calcium in their bones for a prolonged period.
The increased level of parathyroid hormone circulating in our blood causes high amounts of calcium to be released from our bones. This can cause weakness and ‘thinning’ of our bones – a condition known as osteopenia or, if more severe, osteoporosis.