King’s researchers collaborated with doctors at King’s College Hospital NHS Foundation Trust to successfully employ a revolutionary robot system to improve therapy for chronic eye diseases. The custom-built robot was utilized to treat wet neovascular age-related macular degeneration (AMD) by providing a single, less intrusive dosage of radiation, followed by routine injections into the patients’ eyes.
The landmark trial, published in The Lancet, discovered that patients required fewer injections to adequately control the condition, possibly saving approximately 1.8 million injections each year worldwide.
Wet AMD is a devastating eye condition in which aberrant new blood vessels form in the macula, the light-sensing layer of cells at the back of the eyeball. The vessels then begin to bleed blood and fluid, usually resulting in a sudden, permanent, and severe loss of sight.
We discovered that the savings from providing fewer injections are more than the cost of robot-controlled radiotherapy. This innovative treatment can thereby save the NHS money, which can be utilized to treat other patients, while controlling patients’ AMD just as effectively as normal care.
Dr Helen Dakin
AMD affects around 196 million people worldwide, with the Royal College of Ophthalmologists estimating that it affects over 700,000 people in the United Kingdom. The number of people with AMD is predicted to rise by 60% by 2035 as the country’s population ages.
Wet AMD is now treated with frequent injections into the eyeball. Initially, therapy significantly improves the patient’s vision. However, because the injections do not cure the illness, fluid will eventually accumulate again in the macula, necessitating long-term, recurring injections. Most patients require an injection every 1-3 months, and eye injections, which cost between £500 and £800 each, have become one of the most popular NHS operations.
The new treatment is significantly more targeted than conventional procedures, directing three beams of highly focused radiation into the damaged eye. Researchers discovered that individuals receiving robotic radiation required fewer injections to control their condition than patients receiving traditional treatment.
The study found that the robotically controlled device saves the NHS £565 for each patient treated over the first two years, as it results in fewer injections.
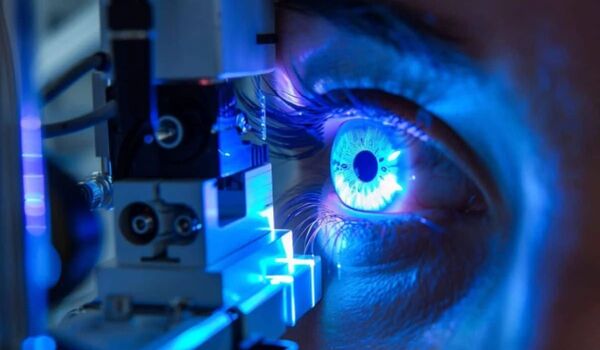
The study lead and first author on the paper, Professor Timothy Jackson, King’s College London and Consultant Ophthalmic Surgeon at King’s College Hospital said: “Research has previously tried to find a better way to target radiotherapy to the macula, such as by repurposing devices used to treat brain tumours. But so far nothing has been sufficiently precise to target macular disease that may be less than 1 mm across.
“With this purpose-built robotic system, we can be incredibly precise, using overlapping beams of radiation to treat a very small lesion in the back of the eye.
“Patients generally accept the need for eye injections to help preserve their vision, but frequent hospital visits and repetitive eye injections are not something they enjoy. The novel medication has the potential to minimize the number of injections required by around a quarter by better stabilizing the condition and decreasing its activity. Hopefully, this discovery helps minimize the treatment load that patients have to bear.”
Dr Helen Dakin, University Research Lecturer at the University of Oxford, stated: “We discovered that the savings from providing fewer injections are more than the cost of robot-controlled radiotherapy. This innovative treatment can thereby save the NHS money, which can be utilized to treat other patients, while controlling patients’ AMD just as effectively as normal care.”
The research was jointly funded by the National Institute for Health and Care Research (NIHR) and the Medical Research Council (MRC) and recruited 411 participants across 30 NHS hospitals. A Lancet-commissioned commentary that accompanied the article described it as a “landmark trial.”