Ongoing research is being conducted on posttraumatic brain activity and its potential association with resilience to post-traumatic stress disorder (PTSD). While I cannot provide the most recent advances on this topic beyond my knowledge cutoff date of September 2021, I can provide you with a general overview of the concept as well as some essential aspects to consider.
PTSD resilience is a complicated and diverse phenomenon that most likely involves a combination of genetic, neurological, psychological, and environmental components. The presence of posttraumatic brain activity is only one piece of the puzzle.
Most people recover without incident after a traumatic encounter, but between 2% and 10% acquire posttraumatic stress disorder (PTSD), a mental health illness that can produce chronic anxiety symptoms owing to emotional dysregulation. In the immediate aftermath of trauma, PTSD symptoms are present in up to 40% of trauma survivors, although full-blown PTSD develops in only a tiny subgroup of instances. Identification of people at risk at an early stage is crucial for both early treatment and possible prevention.
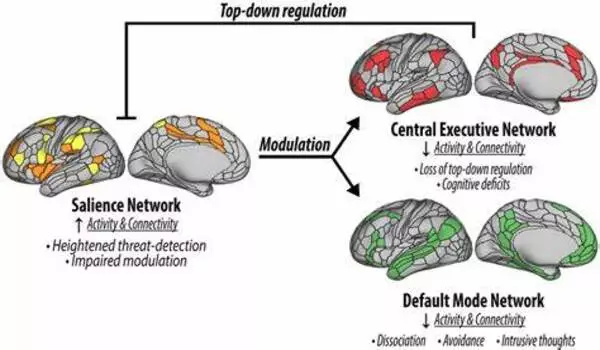
Understanding brain circuits linked to the progression of PTSD from an acute to a chronic condition is critical for understanding its pathophysiology, and ultimately for the development of mechanism-informed treatment.
Dr. Liberzon
A recent study at Texas A&M University conducted by Israel Liberzon, MD, attempted to achieve precisely that. Elsevier publishes the work in Biological Psychiatry: Cognitive Neuroscience and Neuroimaging.
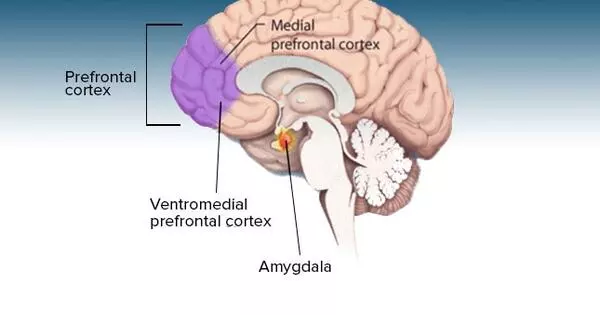
Researchers have long suspected that PTSD involves abnormal brain activity in areas related with emotion processing and modulation, such as the amygdala, insula, and prefrontal cortex. However, it is unclear when the PTSD-related changes appear. The researchers gathered brain scans from 104 survivors of trauma (often a vehicle accident) at 1, 6, and 14 months after the accident for this study. By examining brain activity so soon after the incident, the researchers hoped to find markers of who might be more vulnerable or robust to developing chronic PTSD.
“In this largest-to-date, prospective study of early post-trauma survivors, greater activation in the right inferior frontal gyrus, a region linked to cognitive control and emotional reappraisal, predicts better recovery from early PTSD symptoms,” stated Dr. Liberzon. These findings underscore the critical involvement of cortical/cognitive areas in fear modulation and the development of PTSD.”
Importantly, the researchers observed variations in the patients’ brain activity over time, indicating a continuing, possibly degenerative process.
According to Cameron Carter, MD, Editor of Biological Psychiatry: Cognitive Neuroscience and Neuroimaging, “These findings highlight the key role that the prefrontal cortex may play in conferring resilience to the harmful effects of trauma, through its function representing contextual information and regulating emotional responses.”
“Understanding brain circuits linked to the progression of PTSD from an acute to a chronic condition is critical for understanding its pathophysiology, and ultimately for the development of mechanism-informed treatment,” Dr. Liberzon noted. The findings may also aid doctors in identifying and treating early trauma survivors who are at a higher risk of developing chronic PTSD a year after the traumatic incident.”