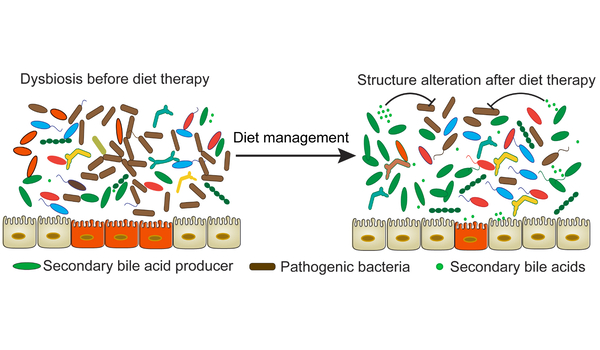
In recent years, there has been an increase in interest in research on the relationship between nutrition and alterations in the microbiome. The human microbiome refers to the enormous collection of microorganisms that inhabit the human body, including bacteria, fungi, viruses, and other microbes, with a high concentration in the gut. According to new research, intermittent fasting and calorie restriction alter the microbiome composition in the gut, which may affect other bodily systems.
Maggie Stanislawski, PhD, assistant professor in the University of Colorado Department of Biomedical Informatics (DBMI), is frequently asked, “Should I be taking a probiotic?”
The solution is difficult. Every person’s gut flora is unique, and she believes that many probiotic pills marketed in grocery stores may not adequately improve gut health for everyone. Instead, the researcher, who focuses on the role of the gut microbiome in obesity and cardiometabolic disease, emphasizes the need to cultivate a diverse microbiome.
Stanislawski and colleagues at the CU School of Medicine are investigating the association between dietary changes and the microbiota. Some of this research investigates how changes in gut flora may influence metabolism after a dietary weight loss strategy.
Our findings support the idea that we may see a lot of changes in microbes associated with diet and obesity during weight loss. We also see an abundance of microbes associated with levels of DNA methylation in genes that we know are involved in relevant processes in the body, such as metabolism.
Iain Konigsberg
Daily caloric restriction vs. Intermittent fasting
Stanislawski worked with CU Department of Medicine assistant professor Vicki Catenacci, MD, on a behavioral weight reduction intervention study that compared the effects of two popular weight loss regimens: intermittent fasting and the more traditional strategy of daily caloric restriction.
Stanislawski investigated the effects of the intervention on the participants’ gut microbiota and discovered that both treatments aid in diversifying the microbiome.
Participants in one group were advised to fast three non-consecutive days each week. The participants were instructed to eat around 25% of what they normally eat on fasting days, and then to eat whatever they wanted on non-fasting days. In the second group, participants were asked to cut calories by the same amount every day, roughly 30% of their weight maintenance requirements. During the intervention, participants were also provided behavioral support and advice on how to improve their overall food quality, as well as encouraged to enhance their physical activity levels.
“Dr. Catenacci and her team were aiming to understand intermittent fasting because it’s become really popular, but some clinicians are hesitant to recommend it for weight loss,” Stanislawski says. “This could give people who are trying to lose weight more options. As you might imagine, being able to eat whatever you want on a specific day, such as for a party or social engagement, is really helpful.”
Researchers discovered several alterations in the microbiome of both groups of participants in a pilot study that focused on the first three months of a one-year intervention study.
“There are various measures of the microbiome that we tend to think about,” Stanislawski says. “Alpha diversity is one of them, and these measures represent the diversity of different types of microbes in an environment.” While this is not always the case, a more diversified and robust microbiome is frequently connected with improved health and leanness. This is most likely because a more diversified group of bacteria in your gut means more microbes that can respond to a more diverse set of health impacts.”
“We looked at various measures of alpha diversity that take into account different features of diversity,” she explains. “They all increased significantly in the first three months of this intervention, which is fantastic.” There were no differences in alpha diversity between the two intervention groups when we looked at differences.”
According to the study’s findings, both dietary weight loss regimens are equally effective in terms of microbiome diversity. Similarly, they observed alterations in the general taxonomic organization of the microbiome makeup in both intervention groups.
“This means that you can choose a dietary weight loss strategy that works for you, and either way your microbiome will likely shift and increase diversity,” Stanislawski says.
The gut and beyond
Changes in the microbiome while undergoing dietary changes may play an important role in additional functions of the body as well.
CU researchers Emily Hill, PhD, RDN, in the Department of Pediatrics, and Iain Konigsberg, PhD, in the DBMI, worked with Stanislawski and Sarah Borengasser, PhD, and several other researchers across the CU Anschutz Medical Campus, on a new study using the same behavioral weight loss intervention data.
The researchers examined the relationships between the gut microbiome and blood DNA methylation. DNA methylation, Konigsberg explains, is the dynamic process of addition and subtraction of methyl groups, which are single carbons to cytosines, the C base of DNA.
“It’s one of the multiple epigenetic mechanisms that regulate our genes without directly altering our DNA sequences,” he says. “DNA methylation is a dynamic process, and it impacts the compaction of our DNA and accessibility by regulatory machinery. The idea is that very broadly speaking, increased methylation at gene regulatory regions generally represses expression of those genes.”
“One of the most appealing aspects of epigenetic mechanisms is that they are a means for the environment to act on our genes and our health,” he explains. For example, smoking has a significant impact on DNA methylation.
“You have certain genes whose activity puts you at a higher risk of some type of disease, but they aren’t activated if you live a healthy lifestyle,” Konigsberg adds. “However, if you smoke, they go haywire.”
Participants in the behavioral weight loss intervention research had connections between gut flora and DNA methylation.
“Our findings support the idea that we may see a lot of changes in microbes associated with diet and obesity during weight loss,” adds Konigsberg. “We also see an abundance of microbes associated with levels of DNA methylation in genes that we know are involved in relevant processes in the body, such as metabolism.”
Both DBMI studies shed light on how food affects not only the microbiome and its variety, but also the rest of the body.
“We are able to show these downstream effects in the body that are associated with the gut microbiome – and may even be mediated through the actions of these microbes,” says Konigsberg.
















