Prostate cancer is very common and is one of the leading causes of cancer death. At the same time, prostate cancer grows so slowly in many cases that it has no effect on survival; thus, routine screening is debatable. Because prostate cancer grows slowly, men who do not have symptoms and do not have a 10-year life expectancy should not be offered testing because they are unlikely to benefit. When making screening decisions, consider your overall health status rather than your age alone.
Over the last 15 years, public health officials have lowered their recommendations for the PSA test as a screening tool in order to reduce overdiagnosis and overtreatment of men with low-grade prostate cancer. Weill Cornell Medicine researchers have discovered that, while these efforts have been successful, the incidence of higher-grade disease and metastasis at diagnosis has increased. The findings were published in the Journal of the National Cancer Institute.
“To our knowledge, this is the first study to demonstrate nationally that low-grade prostate cancer is no longer the most commonly diagnosed type of prostate cancer,” said senior author Dr. Jim Hu, the Ronald P. Lynch Professor of Urologic Oncology at Weill Cornell Medicine and director of the LeFrak Center for Robotic Surgery at NewYork-Presbyterian/Weill Cornell Medical Center. “One of the weaknesses of PSA/prostate cancer screening was that it led to over-detection of indolent cancers that would not harm men, subjecting them to anxiety and future testing.”
To our knowledge, this is the first study to demonstrate nationally that low-grade prostate cancer is no longer the most commonly diagnosed type of prostate cancer. One of the weaknesses of PSA/prostate cancer screening was that it led to over-detection of indolent cancers that would not harm men, subjecting them to anxiety and future testing.
Dr. Jim Hu
The US Preventive Services Task Force (USPSTF) recommended against screening all men with the PSA test in 2012, concluding that the benefits of the test, which measures levels of a protein frequently overproduced in prostate cancer cells, outweighed the risks. The USPSTF then issued a revision in 2018 to include shared decision making for the PSA test for men aged 55 to 69 years, reflecting emerging evidence of longer-term benefits and widespread adoption of active surveillance after low-risk disease detection.
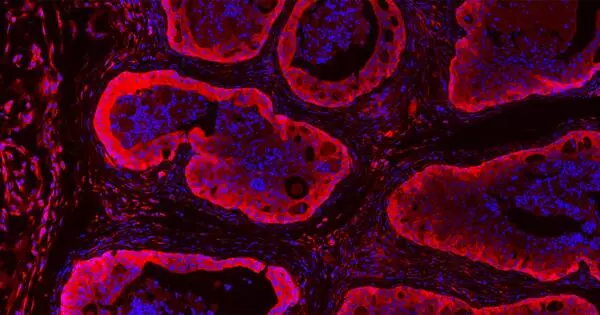
Dr. Hu and colleagues used a nationally representative database to identify more than 438,000 men with newly diagnosed prostate cancer between 2010 and 2018. They used several measures to examine trends in the incidence of prostate cancer by disease risk. The Gleason Grade, a pathology score based on the microscopic appearance of the prostate cells determined at biopsy and after radical prostatectomy, a procedure in which the entire prostate is surgically removed, was one measure.
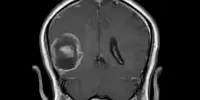
PSA level and presence of metastasis at diagnosis were additional measures. They also looked into whether rising obesity rates or the introduction of newer diagnostic tools like pre-biopsy magnetic resonance imaging (MRI) and biomarkers could explain rising incidence rates.

The analysis revealed a significant decrease in the incidence of the lowest-risk prostate cancer, Gleason Grade 1 (GG1), falling from 52 to 26 cases per 100,000 men across all age groups. Further, the proportion of GG1 found on pathology in men who had a radical prostatectomy decreased from 32 to 10 percent. However, metastases rates at diagnosis increased from 3.0 percent to 5.2 percent over the same period. Halting PSA testing appeared to be the primary driver of these trends.
“The fact that only 10 percent of radical prostatectomy specimens demonstrate low-grade prostate cancer indicates that even when low grade cancer is diagnosed, it is being treated much less frequently, said Dr. Hu. “This demonstrates that there has been acceptance of active surveillance, also known as monitoring with curative intent, among doctors and patients nationally.”
“It’s encouraging to see that urologists in the United States have moved away from overuse of radical therapies for the management of low-risk prostate cancer,” first author Dr. Leonardo Borregales added.
The authors concluded that public health officials should consider implementing risk-stratified screening, such as MRI or biomarkers, to continue to minimize overdiagnosis and avoid biopsy in men with low-risk prostate cancer while addressing the rising trends of high-grade and metastatic prostate cancer.