In comparison to older children and adults, newborns and infants have comparatively weak immune systems. Their immune systems are still learning to distinguish between infections and non-pathogens. Columbia University researchers have discovered why kids are prone to recurring attacks of common respiratory infections–but also have a unique armament to fight off novel germs that healthy adults lack.
A pair of new studies headed by Columbia University researchers explain why babies catch so many common respiratory illnesses and identify a specific cluster of immune cells seen only in babies that help them cope with new viruses.
“We know very little about how the immune system develops throughout life, and most of what we know about immune system development in children comes from animal studies,” says Donna Farber, Ph.D., the study’s lead author and immunology expert at Columbia University’s Vagelos College of Physicians and Surgeons. “However, mice develop much faster than humans, and their immune systems differ slightly from ours.”
Farber’s team was able to identify features of immune system development that separate babies from adults by using a treasure of tissue samples from dead juvenile organ donors.
We discovered that memory T cells in young children are not functionally mature and only begin to have the capacity for protective immunity around the age of 4 to 6 years. This explains why babies and young children are more vulnerable to recurring respiratory infections and other infectious diseases than adults.
Donna Farber
Immune cells in lungs and gut take time to mature
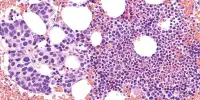
According to one study published in Immunity, specialized immune cells known as memory T cells increase fast in the lungs and intestines through age 3 and more gradually in blood and lymph tissues. These cells let older children and adults to develop a quick and particular immune response when they come into contact with a disease.
But there’s a problem.
“We discovered that memory T cells in young children are not functionally mature and only begin to have the capacity for protective immunity around the age of 4 to 6 years,” Farber explains. “This explains why babies and young children are more vulnerable to recurring respiratory infections and other infectious diseases than adults.”
The findings also may explain why introducing foods to children during the first year of life could prevent severe food allergies. “Early memory T cells are more tolerant than mature memory cells, so they’re not going to create an immune response against new foods,” Farber says.
‘Secret weapon’ protects babies from new pathogens
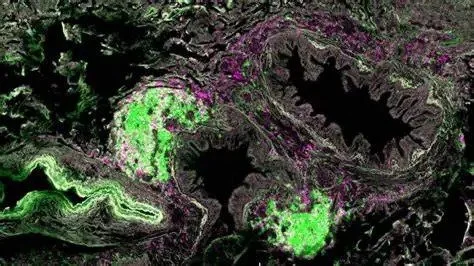
While babies are vulnerable to recurring infections, a second study published in Nature Immunology discovered that they had a unique manner of dealing with novel viruses. In the newborns’ lungs, the researchers discovered clusters of antibody-producing B cells surrounded by T cells. This bronchus-associated lymphoid tissue, or BALT, develops between the ages of 6 and 12 months and fades after the age of 3.
“BALT enables the lung to make antibodies to respiratory pathogens well before T cell memory has developed, but they fall apart in later childhood when they are no longer needed,” Farber explains. “This mechanism helps young children respond to the many different respiratory pathogens they encounter early in life.”
It also may explain why young kids are more resilient to new respiratory infections compared to adults – including SARS-CoV-2.
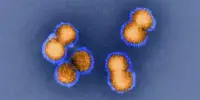
“With SARS-CoV-2, a virus no one had ever encountered before, we saw that people in their 50s and 60s were very susceptible to severe COVID, but most kids exposed to SARS-CoV-2 were fine, and many didn’t even have symptoms,” Farber explains. “We concluded that babies and young children must have adaptations to respond to new pathogens that adults do not.”
BALT may possibly play a role in the development of persistent asthma and allergies in some children. “It’s possible that these diseases are caused in part by BALT’s abnormal persistence well into childhood, which could trigger an overreaction to certain antigens,” Farber adds.
Farber adds that the study could explain why early trials of intranasal COVID vaccines failed to show promise in adults while intranasal influenza vaccination works better in youngsters. “It could be that this type of vaccine works better in children because they have BALT structures that can initiate new antibodies in the lungs.”
“BALT provides some protection, but it clearly does not protect young children from everything,” Farber adds. “We must remember that prior to vaccines, one-third of children died from infectious diseases in infancy.” As a result, childhood immunizations are critical for our protection.”