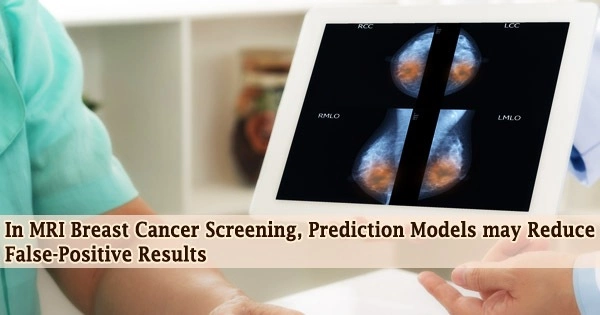
According to a recent study published in the journal Radiology, prediction models based on clinical traits and imaging results may help lower the false-positive rate in women with dense breasts who receive further breast cancer screening with MRI.
Compared to women with typical breast density, individuals with dense breast tissue have a significantly increased risk of developing breast cancer. Due to the fibroglandular tissue’s masking effect, high breast density also significantly lowers the sensitivity of mammography, which means that malignancies may be concealed within dense breast tissue.
For women with dense breast tissue, breast MRI is regarded as a potentially beneficial addition to mammography screening. It is the most accurate imaging method for detecting breast cancer and does a good job of distinguishing between lesions and breast anomalies.
Its significant increased value as a screening tool for women at high risk of breast cancer has been proven by research. However, because of its high sensitivity, MRI is a great screening technique since it frequently picks up benign tumors that could not have been seen otherwise.
Women who are referred back for extra testing as a result of these findings may have to have targeted ultrasonography, another MRI scan, and a biopsy. Additional research may be required, which could make the patient more anxious, cost more to treat, or result in difficulties with the biopsy itself.
“The reduction of the false-positive recall rate is an important issue when considering the use of breast MRI as a screening tool,” said study lead author Bianca M. den Dekker, M.D., from the University Medical Center Utrecht in Utrecht, the Netherlands.
Our prediction models may identify a substantial number of false-positives after first-round supplemental MRI screenings, reducing false-positive recalls and benign biopsies without missing any cancers. This brings supplemental screening MRI for women with dense breasts one step closer to implementation.
Bianca M. den Dekker
Dr. den Dekker and colleagues used prediction models in the new study to distinguish between true-positive MRI screening results and false-positive results. They integrated MRI results with clinical traits like body mass index, family history of breast cancer, and usage of hormone replacement treatment to develop the models.
They analyzed information from the Dense Tissue and Early Breast Neoplasm Screening (DENSE) experiment, which examined Dutch breast cancer screening participants aged 50 to 75 who had exceptionally dense breasts to see how well mammography + MRI performed compared to mammography alone.
In the first supplemental MRI screening round, 454 women received positive MRI results; however, only 79 of them were later found to have breast cancer, leading to 375 false-positive MRI tests.
Without missing any tumors, the comprehensive prediction model, based on all gathered clinical data and MRI results, may have avoided 45.5% of false-positive recalls and 21.3% of benign biopsies.
A 35.5% reduction in false-positive MRI screenings and a 13.0% reduction in benign biopsies might have been achieved by using a model that was only based on age and easily accessible MRI data.
“Our prediction models may identify a substantial number of false-positives after first-round supplemental MRI screenings, reducing false-positive recalls and benign biopsies without missing any cancers,” Dr. den Dekker said. “This brings supplemental screening MRI for women with dense breasts one step closer to implementation.”
Utilizing information from various demographics, the researchers plan to carry out validation tests. Additionally, they aim to research how well prediction models function in subsequent screening rounds.
In the research group, the false-positive rate decreased from 79.8 per 1,000 screenings in the first round to 26.3 per 1,000 in the second, according to Dr. den Dekker.
“This can be partly explained by the availability of prior MRI examinations, which allows comparison for interval change,” she said. “As incident screening rounds have a much lower false-positive rate, separate models may have to be created.”