Researchers at the University of British Columbia have demonstrated for the first time how and why drugs can deplete bacteria in a newborn’s gut, resulting in lifelong respiratory allergies.
In a study published in the Journal of Allergy and Clinical Immunology, a research team from the School of Biomedical Engineering (SBME) found a unique chain of events that leads to allergies and asthma. In doing so, they have created numerous new pathways for investigating potential preventions and therapies.
“Our research finally shows how the gut bacteria and antibiotics shape a newborn’s immune system to make them more prone to allergies,” said senior author Dr. Kelly McNagny (he/him), professor in the SBME and the department of medical genetics. “When you see something like this, it really changes the way you think about chronic disease. This is a well-sculpted pathway that can have lasting consequences on susceptibility to chronic disease as an adult.”
We can now detect when a patient is on the verge of developing lifelong allergies, simply by the increase in ILC2s. And we can potentially target those cell types instead of relying on supplementation with butyrate, which only works early in life.
Ahmed Kabil
Allergies are caused by the immune system responding too strongly to harmless items such as pollen or pet dander, and they are the primary cause of emergency room visits in children. Normally, the immune system defends us against hazardous invaders such as bacteria, viruses, and parasites. In the case of allergies, it misidentifies something harmless as a threat — in this example, parasites — and initiates a response that causes symptoms such as sneezing, itching, or swelling.
Our immune system’s development begins very early in life. Microbes in the baby gut appear to play an important role, according to research conducted over the last two decades. Antibiotics are frequently administered to babies shortly after birth to fight illnesses, which can reduce the number of specific bacteria. Some of these bacteria create a chemical called butyrate, which is critical for stopping the mechanisms discovered in this study.
Dr. McNagny’s lab previously demonstrated that infants with less butyrate-producing bacteria are more sensitive to allergies. They also demonstrated that this could be minimized or even reversed by administering butyrate as a supplement early in life.
Now, by studying the process in mice, they have discovered how this works.
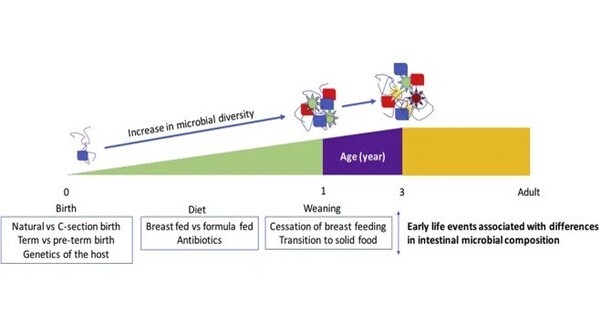
Mice with reduced gut bacteria who did not get a butyrate supplement generated twice as many ILC2s. These cells, discovered less than 15 years ago, have quickly become leading suspects in allergy development. The researchers discovered that ILC2s create chemicals that ‘turn the switch’ on white blood cells, causing them to manufacture an abundance of specific types of antibodies. These antibodies then coat cells to protect them from external invaders, providing the allergic person with an immune system that is ready to fight at the slightest provocation.
Without butyrate to suppress them, the number of each cell, molecule, and antibody outlined in this cascade increases substantially.
Butyrate must be given during a narrow window after birth — a few months for humans, a few weeks for mice — in order to prevent the proliferation of ILC2s and all that follows. If that opportunity is missed and ILC2s multiply, then the remaining steps are assured and remain with somebody for life.
Now that researchers know what those other steps are, they have many more potential targets for halting the cascade, even after the supplementation window has closed.
“We can now detect when a patient is on the verge of developing lifelong allergies, simply by the increase in ILC2s,” said Ahmed Kabil (he/him), the study’s first author and a PhD candidate in the SBME. “And we can potentially target those cell types instead of relying on supplementation with butyrate, which only works early in life.”
According to Dr. McNagny and study co-leader Dr. Michael Hughes, treating people’s allergies with antihistamines and inhalers just reduces symptoms, not curing the disease. To make more long-term progress, researchers must target the cells and systems that comprise this hypersensitive immune system. There had previously been no method to accomplish this selectively.
With this new understanding, patients can look forward to more effective, long-term therapies that target the underlying cause of the disease, opening the way for a future in which allergies are better managed, if not eliminated entirely.