In children, brain inflammation, commonly known as encephalitis, can cause neurological abnormalities. Encephalitis is an inflammation of the brain tissue caused by a variety of factors such as viral infections, autoimmune reactions, and others.
Severe inflammation in childhood is a clinically recognized risk factor for autism and schizophrenia. For the first time, researchers at the University of Maryland School of Medicine (UMSOM) have identified that inflammation changes the formation of susceptible brain cells, which may have mechanistic implications for neurodevelopmental diseases. This discovery could pave the way for treatments for a wide range of childhood-onset neurodevelopmental diseases.
Researchers from the University of Maryland School of Medicine led a study that discovered inflammation in early childhood prevents specific neurons in the cerebellum from maturing completely. They used single-cell genomics to study the brains of children who died from inflammatory conditions such as bacterial or viral infections or asthma, as well as those who died in a sudden accident. The cerebellum is a brain region that is in charge of physical control as well as higher cognitive processes such as language, social skills, and emotional regulation.
The study was carried out by faculty from UMSOM’s Institute for Genome Sciences (IGS), Department of Pharmacology, and the University of Maryland-Medicine Institute of Neuroscience Discovery (UM-MIND). The findings are published in the October issue of Science Translational Medicine. It is one of roughly 30 articles that describe the growth and diversity of cell types in the human brain. The Brain Research Through Advancing Innovative Neurotechnologies (BRAIN) Initiative Cell Census Network, a multisite consortium supported by the National Institutes of Health, coordinated all of these investigations.
This study is one of the first to show that changes in gene expression during inflammation may set the stage for later cellular dysfunction, such as reducing synaptic connectivity or altering energy metabolism.
Dean Mark Gladwin
Previous research has shown that babies born with abnormalities of the cerebellum frequently go on to experience neurodevelopmental disorders, and animal models exposed to inflammation before birth also develop these conditions.
“We looked at the cerebellum because it is one of the first brain regions to develop and one of the last to mature,” said Seth Ament, Ph.D., IGS scientist and Associate Professor in the Department of Psychiatry at UMSOM, who co-led the research with Margaret McCarthy, Ph.D., James and Carolyn Frenkil Dean’s Professor and Chair in Pharmacology and Director of UM-MIND. “With the fairly new technology of single nucleus RNA sequencing we could look at the cell level to see changes in the brains.”
“This has never been done before in this age group and in the context of inflammation,” Dr. McCarthy added. In children with inflammation, gene expression in the cerebellum was astonishingly constant.”

The researchers studied donated post-mortem brain samples from 17 infants who died between the ages of one and five, eight from inflammatory disorders and nine from accidents. Prior to death, none of the donors had been diagnosed with a neurological disease. Age, gender, race/ethnicity, and time since death were all comparable between the two groups. These one-of-a-kind brain tissue specimens were gathered over many years by UMSOM researchers at the University of Maryland Brain and Tissue Bank, the Maryland Psychiatric Research Center’s Maryland Brain Collection, and the NIH NeuroBioBank in Bethesda, Maryland.
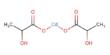
The Golgi and Purkinje neurons were shown to be the most sensitive to brain inflammation in the study, despite their rarity. These two classes of neurons revealed early interruption of development at the single-cell level.
“Although rare, Purkinje and Golgi neurons have critical functions,” according to Dr. Ament. “During development, Purkinje neurons form synapses that connect the cerebellum to other brain regions involved in cognition or emotional control, while Golgi neurons coordinate communication among cerebellar cells.” Inflammation may contribute to illnesses such as autism spectrum disorders and schizophrenia if either of these developmental pathways is disrupted.”
As with many diseases, both genetics and the environment — in this case, inflammation — likely contribute to the risk of developing these disorders. That’s why it is crucial to understand the roles of specific cells within the brain regions — as well as how they interact with genes to influence brain function — to find treatments for brain disorders, like ASD and schizophrenia, as well as others including dementia, Parkinson’s disease, or substance use disorders.
“This study is one of the first to show that changes in gene expression during inflammation may set the stage for later cellular dysfunction, such as reducing synaptic connectivity or altering energy metabolism,” said UMSOM Dean Mark Gladwin, M.D., who is also Executive Vice President for Medical Affairs at UM Baltimore and the John Z. and Akiko K. Bowers Distinguished Professor at UMSOM. “It’s critical to understand these mechanisms and changes at the cellular level during brain development in the hope that someday we can develop treatments for neurodevelopmental disorders.”