Acute otitis externa, often known as swimmer’s ear, is among the most typical ear infections that affect both children and adults.
Swimmer’s ear will affect about 10% of Americans at some point in their lives. Children, typically between the ages of 5 and 12, are infrequently afflicted while adults are more frequently.
But swimmer’s ear can occur even while you are not swimming. On a hot day, if you go for a jog, a walk, or do yard work, perspiration may drip into your ears. The ailment is known as “swimmer’s ear” because swimmers are five times more likely to experience it. Additionally, because of the humidity and greater temperatures in tropical settings, it happens more frequently.
We are actively engaged in clinical care for children and adults with ear, nose, and throat issues as ear specialists who conduct clinical research. We have undoubtedly seen our fair share of swimmer’s ear patients while operating in the state of Florida.
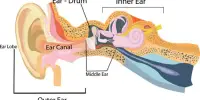
Symptoms and causes of swimmer’s ear: An infection of the external ear canal, which connects the ear opening to the eardrum, is known as swimmer’s ear. Swimmer’s ear typically affects just one ear, although occasionally the eardrum itself is impacted. The skin barrier breaks down as a result of moisture trapped in the canal, allowing new forms of bacteria to enter or existing ones to overgrow.
The bacterium Pseudomonas aeruginosa, which is found in soil and water all around the world, is one of these causes. These microorganisms prefer wet locations like sinks, toilets, poorly chlorinated hot tubs, and swimming pools, as well as old or ineffective antiseptic cleaners.
You will be aware if you are infected. Generally, symptoms start to show up a few days after infection. Severe pain and discomfort are the primary signs and symptoms of swimmer’s ear. It’s especially obvious when the outer ear is pulled or when you touch the tragus, the tiny protrusion at the front of your ear. Redness, swelling, discharge, and irritation inside the ear are other symptoms. Along with imbalance issues, transient hearing loss, and a sense of fullness, these symptoms are also sometimes accompanied by the perception of a blocked ear.
vulnerability to the swimmer’s ear: Swimmer’s ear can be caused by a variety of circumstances. They include having a small ear canal and having skin conditions like psoriasis or eczema. Additionally, people who use earbuds, earplugs, or hearing aids may be at a higher risk. Also more vulnerable to the virus may be diabetics.
In addition to getting something lodged inside the ear, over-cleaning the ears, or coming into touch with chemicals from hair dye or hairspray can also cause swimmer’s ear.
Identification and treatment: The diagnosis of swimmer’s ear follows a detailed medical history inquiry and internal ear examination. Usually, the ear canal will appear red, bloated, and damp. The sight of fluid drainage or scaly, peeling skin is another potential. The eardrum could be difficult to see, depending on how much swelling there is. It is possible to take a sample of ear fluid and send it to a lab to be examined for bacteria or fungus.
Swimmer’s ear is frequently treated with eardrops. Antibiotics to treat the infection and medications to reduce edema are frequently included in these drops.
Ciprodex is a sample of an eardrop. It comprises the strong steroids dexamethasone and the antibiotic ciprofloxacin. Patients must administer four to five drops twice daily for seven to ten days into the infected ear canal.
Floxin, another often administered drop, includes an antibiotic but no steroids. It is frequently used for ears that are infected but less swollen.
Other drop preparations include Cortisporin, which contains hydrocortisone as well as a regularly used combination of neomycin and polymyxin B. However, because neomycin can also harm the inner ear, medical professionals now frequently prescribe Ciprodex or Floxin instead.
A wick or stent may be inserted by the doctor into the ear canal to keep it open in cases where the ear canal is too enlarged for drops to reach the diseased area. The doctor will typically leave this in place for three to five days before removing it, although occasionally the wick will come out once the swelling goes down. Usually, the infection is gone and the skin of the ear canal returns to normal after 10 days.
Taking care of an ongoing infection: After using eardrops for seven to ten days to treat swimmer’s ear, it may occasionally still persist. If the infection has migrated outside of the ear canal or in patients with poorly managed diabetes, oral antibiotics are frequently advised. Although hospitalization is not frequently required for swimmer’s ear, certain problems, such as fever, increasing discharge, significant ear canal narrowing, or failure of prior therapies, may do so.
The following are some measures you can take to avoid a swimmer’s ear: Dry out the ear canal. To help the water drain, tilt your head to one side. Use a soft cloth or towel, or use a hair dryer sparingly close by.
A doctor should clean the ear canal if the ear canal’s self-cleansing system is compromised.
Reducing the pH in the ear canal helps stop bacterial overgrowth because the majority of bacteria prefer a pH-neutral environment. A homemade liquid tincture can be created by combining equal parts distilled white vinegar and rubbing alcohol. The alcohol in the ear mixes with the water there before evaporating. Water is removed while bacteria are prevented from developing by the vinegar’s acidity.
When used as a preventative precaution soon after the ear has been exposed to wetness, two to three drops are typically adequate. This liquid remedy should only be used by those who are predisposed to ear infections due to prolonged or repeated exposure to moisture. It is not intended to replace medical therapy for genuine ear infections.
Additionally, it’s critical to distinguish between swimmer’s ear and a middle ear infection, which accounts for the majority of antibiotic prescriptions given to children under the age of 5. Middle ear infections frequently occur during the fall and winter, when influenza and cold viruses are more common, and they are typically accompanied by viral upper respiratory illnesses.