Researchers have developed a low-cost, RNA-based technology for detecting and measuring biomarkers, which can aid in decoding the physiology of the body. Protein biomarkers can indicate chronic or acute conditions ranging from arthritis to cancer to bacterial infections, and conventional tests can cost anywhere from $100 to $1,000. The same measurement can now be performed for less than a dollar using new technology.
Penn State researchers have developed a low-cost RNA-based technology for detecting and measuring biomarkers, which can aid in the decoding of the body’s physiology. Protein biomarkers can indicate chronic or acute conditions ranging from arthritis to cancer to bacterial infections, and conventional tests can cost anywhere from $100 to $1,000. The same measurement can now be performed for less than a dollar using new technology.
The team published their results in Nature Communications, combining the efforts of Howard Salis, associate professor of biological engineering, chemical engineering and biomedical engineering; Grace Vezeau, who earned a doctorate in biological engineering from Penn State in 2021; and Lipika Gadila, who earned a bachelor of science in chemical engineering from Penn State in 2018.
Currently, assays require expensive detection reagents, expensive and bulky instruments, sample cold chain storage and distribution, and trained personnel. We engineered low-cost protein sensors that can be freeze-dried and rehydrated using modeling and computational design.
Howard Salis
The findings show that RNA-based sensors can be programmed to detect human biomarker proteins such as monomeric C-reactive protein, which is involved in chronic inflammatory conditions such as heart disease and arthritis, and interleukin-32 gamma, a signaling protein involved in acute infections such as viruses or bacterial infections. According to Salis, such sensors could be used to create diagnostic testing devices.
“These tests can assist a clinician in diagnosing a patient, but it’s more informative to perform multiple biomarker measurements on a regular basis over the course of several weeks,” Salis said. “Right now, a single test can be costly, and they add up. With our new RNA-based technology, we can now perform the same measurements for much less.”
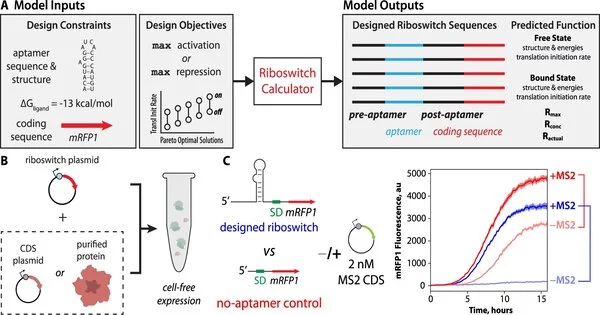
The technology combines a cell-free expression system with engineered RNA-based sensors known as riboswitches. Cell-free expression systems have cellular machinery to read DNA and produce proteins, but they are not restricted by cell membranes and can therefore accept bulky proteins. Riboswitches are designed to bind to biomarker proteins and control the activation or repression of an observable signal. The riboswitch is created within the cell-free expression system using DNA instructions. The total cost of these materials is approximately one dollar per reaction.
According to Salis, this is the first time that researchers have engineered a riboswitch sensor to detect biomarker proteins. The challenge, he said, is figuring out the best DNA instructions to generate the most sensitive protein sensors.
“Past efforts to engineer such riboswitch sensors have largely relied on trial-and-error experimentation, for example, constructing and characterizing large random libraries to identify riboswitch variants – the genetic blueprints and aptamers – that work best,” Salis explained. “We rationally designed new riboswitches that are predicted to be excellent protein sensors using a combination of thermodynamic modeling and computational optimization, and then tested them. The Riboswitch Calculator is the name of our design algorithm.”
As a proof-of-principle test, Salis and colleagues used MS2, a small protein found in a bacterial phage, as well as the medically relevant biomarkers human monomeric C-reactive protein and human interleukin-32 gamma. The scientists created 32 riboswitches, the majority of which successfully sensed their target proteins.
“Currently, assays require expensive detection reagents, expensive and bulky instruments, sample cold chain storage and distribution, and trained personnel,” Salis explained. “We engineered low-cost protein sensors that can be freeze-dried and rehydrated using modeling and computational design. The next step is to create a user-friendly device that will allow researchers and clinicians to use this new technology.”
Salis is also a member of Penn State’s Institutes of Energy and Environment.