The development of an artificial kidney that can completely replace the need for dialysis in patients with end-stage renal disease (ESRD) was still a work in progress. However, there have been significant advancements in the field of artificial kidneys and renal replacement therapies, and I can provide some insights into the state of research up to that point.
Scientists at UC San Francisco are developing a new strategy to treating kidney failure that could one day eliminate the need for dialysis or the use of harsh medicines to suppress the immune system following a transplant.
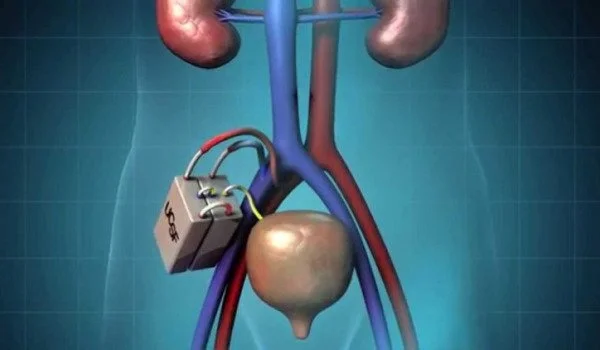
They demonstrated for the first time that kidney cells housed in a bioreactor, an implanted device, can live within the body of a pig and replicate numerous critical kidney processes. The gadget, like a pacemaker, can operate silently in the background and does not activate the recipient’s immune system.
The findings, published in Nature Communications, are an important step forward for The Kidney Project, which is jointly headed by UCSF’s Shuvo Roy, PhD (technical director) and Vanderbilt University Medical Center’s William H. Fissell, MD (medical director).
We are focused on safely replicating the key functions of a kidney. The bioartificial kidney will make treatment for kidney disease more effective and also much more tolerable and comfortable.
Shuvo Roy
Scientists hope to eventually fill the bioreactor with diverse kidney cells that perform important activities such as fluid balance and hormone release to regulate blood pressure, and then pair it with a device that filters waste from the blood.
The goal is to create a human-scale gadget that will improve on dialysis, which keeps people alive after their kidneys fail but is a poor alternative for having an actual functioning organ. Over 500,000 people in the United States require dialysis multiple times per week. Many patients want kidney transplants, but there aren’t enough donors, so only approximately 20,000 people get them each year. A transplantable kidney would be a godsend.
“We are focused on safely replicating the key functions of a kidney,” said Roy, a bioengineering professor in the UCSF School of Pharmacy. “The bioartificial kidney will make treatment for kidney disease more effective and also much more tolerable and comfortable.”
Inspired by nature, honed by science
Roy and his colleagues designed the bioreactor to link directly to blood vessels and veins, allowing nutrients and oxygen to pass through, much like a donated kidney. Silicon membranes protect the kidney cells inside the bioreactor from immune cell attack.
As a test case, the researchers employed a type of kidney cell called a proximal tubule cell, which regulates water. H. David Humes, MD, of the University of Michigan, who co-authored the study, had previously utilized these cells to aid dialysis patients in the intensive care unit, with life-saving effects.
A green light for The Kidney Project
Both the kidney cells and the recipient mice did well after transplantation, according to the researchers. The next phase will be month-long testing in animals, followed by human trials, as mandated by the US Food and Drug Administration (FDA).
“We needed to demonstrate that a functional bioreactor does not require immunosuppressive drugs,” Roy stated. “There were no complications, and we can now iterate, aiming for the entire panel of kidney functions on a human scale.”