New research suggests that MRI scans could replace invasive heart testing by correctly estimating pressures inside the heart and predicting whether a patient would develop heart failure.
The University of East Anglia (UEA) and Queen Mary University of London conducted research that identified important risk factors for increasing pressure inside the heart, which leads to heart failure. These risk factors include being over 70, having high blood pressure, being fat, drinking alcohol, and being male.
Co-lead author Dr Pankaj Garg, from UEA’s Norwich Medical School, said: “Heart failure is a lethal condition resulting from rising pressures. One of the most significant findings of this study is that MRI-derived pressure measurements can reliably predict if an individual will develop heart failure.
“This breakthrough suggests that heart MRI could potentially replace invasive diagnostic tests. Participants with higher heart pressure measured by MRI had a fivefold increased risk of developing heart failure over six years.”
This breakthrough suggests that heart MRI could potentially replace invasive diagnostic tests. Participants with higher heart pressure measured by MRI had a fivefold increased risk of developing heart failure over six years.
Dr Pankaj Garg
Previous pioneering research conducted by UEA and the universities of Sheffield and Leeds demonstrated that heart MRI techniques can estimate heart pressure and are associated with symptoms and indicators of heart failure. However, it remains questionable if heart MRI-derived pressures can predict heart failure risk in the general population.
This current study, which examined data from more than 39,000 UK Biobank participants, found that MRI-detected pressure changes can indicate heart failure risk without invasive procedures.
Co-lead author Dr Nay Aung, from the William Harvey Research Institute at Queen Mary University of London, said: “Additionally, we identified key risk factors for developing high heart pressure: age over 70, high blood pressure, obesity, alcohol consumption and male gender. By combining these factors, we developed a model to predict individual heart failure risk. This advancement enables prevention, early detection and treatment of heart failure, which could save many lives.”
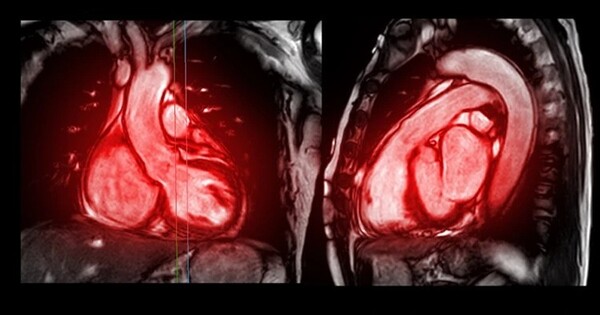
A heart MRI is a type of scan that uses powerful magnets and radio waves to create detailed images of the heart. Unlike X-rays or CT scans, it does not use harmful radiation.
In this research work, both teams analysed heart MRI data from 39,000 UK biobank participants using artificial intelligence techniques and estimated the pressure inside the heart. They then evaluated each individual’s risk factors and their chance of developing heart failure in the future over a six-year follow-up period.
The University of East Anglia conducted the research in collaboration with Queen Mary University of London. Other contributors include St Bartholomew’s Hospital in London, Norfolk and Norwich University Hospitals, the universities of Leeds and Sheffield, Health Data Research UK, and the Alan Turing Institute.
The UK Biobank is a large-scale biomedical database and research resource that contains de-identified genetic, lifestyle, and health information, as well as biological samples from half a million UK individuals. The Wellcome Trust and the National Institute for Health and Care Research (NIHR) provided funding for this study.