Ultrasound technology has been investigated for its potential to treat hypertension by targeting nerves involved in blood pressure regulation. This technique is also known as renal denervation or renal nerve ablation. Some patients might benefit from a device that uses ultrasound to soothe hyperactive nerves in the kidneys.
According to a new study led by Columbia University and the Université of Paris in France, the gadget consistently decreased daytime ambulatory blood pressure by an average of 8.5 points in middle-aged hypertensive adults.
In individuals with hypertension, doctors typically suggest lifestyle adjustments such as lowering salt intake or dropping weight, as well as blood pressure drugs. Despite these measures, around one-third of hypertension individuals are unable to regulate their blood pressure.
“Many patients in our clinical practice are just like the patients in our study, with uncontrolled blood pressure in the 150s despite some efforts,” says Ajay Kirtane, MD, co-leader of the study and professor of medicine at Columbia University Vagelos College of Physicians and Surgeons.
Renal ultrasound could be offered to patients who are unable to get their blood pressure under control after trying lifestyle changes and drug therapy, before these events occur.
Ajay Kirtane
Uncontrolled blood pressure over an extended period of time can result in heart failure, strokes, heart attacks, and irreparable kidney damage.
“Renal ultrasound could be offered to patients who are unable to get their blood pressure under control after trying lifestyle changes and drug therapy, before these events occur,” says Kirtane, an interventional cardiologist and director of cardiac catheterization laboratories at NewYork-Presbyterian/Columbia University Irving Medical Center.
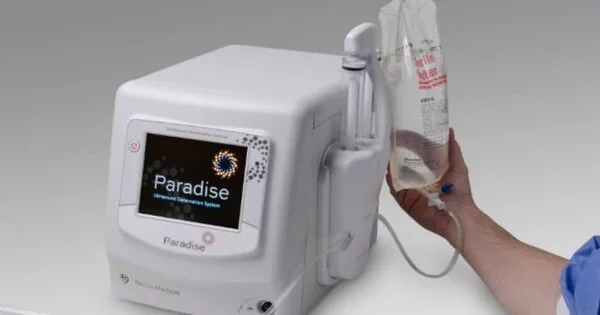
The study’s findings, published in JAMA Cardiology, put the device to the test, which is utilized in an outpatient surgery called ultrasound renal denervation. The device is still experimental, and the FDA has not yet cleared it for usage outside of clinical trials.

Kidney nerves and hypertension
Middle-age hypertension is considered to be caused in part by hyperactive neurons in the kidneys, which induce water and sodium retention and the production of hormones that elevate blood pressure. (As blood arteries stiffen in the elderly, hypertension is more common). Antihypertensive medications lower blood pressure in a variety of ways, including dilating blood vessels, eliminating extra fluid, and blocking hormones that elevate blood pressure. However, none of these drugs directly target the renal nerves.
Ultrasound therapy relaxes hyperactive nerves in the renal artery, interfering with the signals that cause hypertension. A tiny catheter is placed into a vein in the leg or wrist and threaded to the kidney to deliver the therapy to the nerves.
Study results
The new study pooled data from three randomized trials encompassing more than 500 middle-aged patients with varying degrees of hypertension and medication use. Twice as many patients who received the ultrasound therapy reached their target daytime blood pressure (less than 135/85 mmHg) compared to patients in the sham groups.
“The result was almost identical across the different study groups, which definitively shows that the device can lower blood pressure in a broad range of patients,” Kirtane says.
The procedure was well-tolerated, and most patients were discharged from the hospital the same day. According to Kirtane, improvements in blood pressure were seen as soon as one month after the procedure. The treatment will be evaluated by the FDA in the coming months.
Bottom line for patients with resistant hypertension
The researchers believe the treatment might be used in addition to medication and lifestyle changes for people with uncontrolled hypertension. “Once the device is available, we plan to recommend it to patients who have already tried other therapies. The hope is that by controlling blood pressure, we will be able to prevent kidney damage and other side effects of high blood pressure,” Kirtane adds.