According to recent research from the University of Virginia School of Medicine, antidepressant usage during pregnancy may increase the chance of long-term neurodevelopment alterations in kids’ brains, such as those linked to autism.
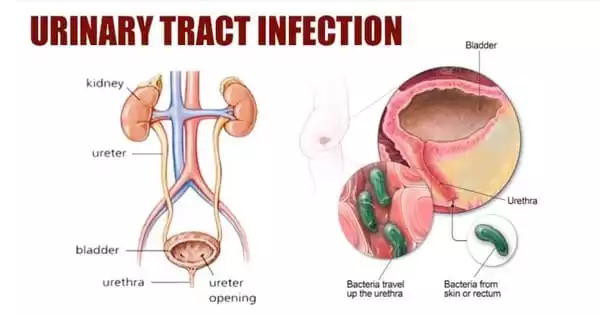
Selective serotonin reuptake inhibitors (SSRIs), a kind of widely prescribed antidepressants, have been found to have potent interactions with the inflammation caused by infections or other causes in the mother’s body. The direct connection between mother and kid, the decidua, was negatively altered in laboratory mice as a result of this interaction, which also had an adverse effect on the growing brain.
“Our findings suggest that SSRIs can have deleterious consequences when mixed with infection, inflammation, etc.,” said senior researcher John Lukens, PhD, of the UVA Department of Neuroscience and its Center for Brain Immunology and Glia (BIG), as well as the UVA Brain Institute. “Our results might help to explain the rise in autism prevalence over the last 20 years, as this time coincides with the rollout of widespread SSRI usage in the developing world.”
SSRIs during Pregnancy
80% of pregnant women who require depression medication are prescribed SSRIs, making them a common choice throughout pregnancy. Although there has been some indication that the medications can raise the risk of premature birth as well as the risk of neurological abnormalities and other health problems in children, they are generally regarded as a safe alternative for controlling depression in pregnant women.
We found that mothers who encountered an immune challenge during pregnancy showed a totally different signature in the placenta when they were on SSRIs compared to mothers that were not on SSRIs. This highlights the importance of considering the entire prenatal environment, as drugs designed to dampen inflammation may lead to unanticipated consequences on the baby if they are combined with other modulators, such as SSRIs.
Kristine Zengeler
The “maternal-fetal interface,” the area where mother and fetus physically touch during pregnancy, is where Lukens and his associates discovered that SSRIs can interact with the mother’s immune system to trigger a potent inflammatory response.
The offspring of mothers who were exposed to inflammation later had sex-based behavioral alterations resembling those in autistic individuals, including lowered social interest and reduced communication. Such mouse models are widely used as an important autism research tool.
“We identified inflammatory signatures in the placenta that correlated with neurologic changes in the adult offspring of mothers that encountered an immune challenge during pregnancy,” said researcher Kristine Zengeler, the first author of a new scientific paper outlining the findings.
“These signatures could be used to help identify biomarkers and druggable targets to help mitigate neurodevelopmental consequences of prenatal environmental stressors, like an immune response.”
Neurodevelopment can be impacted by infections, autoimmune diseases, and other illnesses that influence a mother’s immune system during pregnancy, according to earlier studies. According to UVA researchers, SSRIs may interact with this inflammation, exacerbate it, and cause long-lasting brain alterations.
The researchers claim that because of how SSRIs affect serotonin in the body, the results make sense. Serotonin is a key mood stabilizer and is frequently referred to as the “feel good” molecule in the brain, but it is also an essential immune response regulator.
In the early stages of pregnancy, developing children only receive serotonin from their mothers through the placenta, therefore tampering with mom’s serotonin levels could have negative effects on the unborn child as well.
The researchers discovered that serotonin levels in the placenta were affected by inflammation both on its own and in combination with SSRIs, but in opposing ways.
“We found that mothers who encountered an immune challenge during pregnancy showed a totally different signature in the placenta when they were on SSRIs compared to mothers that were not on SSRIs,” Zengeler said. “This highlights the importance of considering the entire prenatal environment, as drugs designed to dampen inflammation may lead to unanticipated consequences on the baby if they are combined with other modulators, such as SSRIs.”
The researchers underlined that pregnant women shouldn’t discontinue taking SSRIs without first visiting their doctors, noting that they are crucial tools for controlling depression.
Instead, the researchers are urging more research, including involving humans, to ascertain how the medications might impact mother and kid as well as to comprehend how SSRIs interact with inflammation.
“Untreated maternal stress, depression and anxiety can all on their own perturb offspring neurodevelopment, contributing to adverse behavioral and cognitive outcomes,” the researchers write. “It will therefore be of utmost importance to consider both the relative benefits and potential consequences of SSRIs as a therapeutic option during pregnancy.”
Findings Published
The researchers have published their findings in the scientific journal Brain, Behavior and Immunity. The team consisted of Zengeler, Daniel A. Shapiro, Katherine R. Bruch, Catherine R. Lammert, Hannah Ennerfelt and Lukens. The researchers reported no financial interests in the work.
Another new finding from Lukens’ group may hold the key to strengthening the brain’s resistance to multiple sclerosis and Alzheimer’s disease.