In the United States, there is little evidence of a link between structural racism and mortality. We looked at the relationship between ongoing structural racism and disparities in adulthood income between White and Black children with similar parental household income (economic mobility gap) in a recent birth cohort, as well as disparities in death rates (mortality gap) overall and for major causes.
A new study finds that structural racism, as measured by the racial economic mobility gap between Black and White people with similar parental income (as an indicator of similar childhood socioeconomic status), is strongly associated with Black-White mortality disparities in the United States, both in a recent birth cohort and across all ages. These findings, published in Cancer Epidemiology, indicate that the effects of structural racism on mortality have persisted to a similar magnitude across generations over the last century.
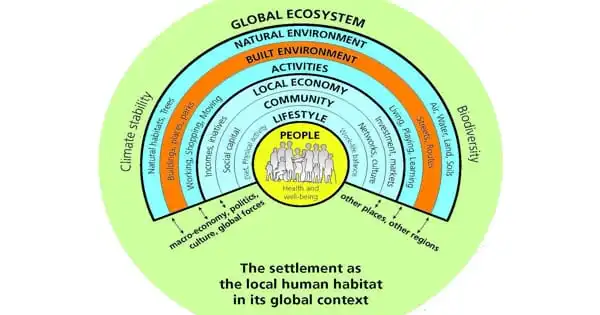
Social inequalities and discriminatory policies based on race/ethnicity, also known as structural racism, are major contributors to health disparities. Structural racism can have a negative impact on the economic, social, service, and physical living environments, resulting in fewer educational and job opportunities, lower-income, poorer housing, transportation, and public safety, food insecurity, and limited health care.
While more research is needed to identify factors mediating these associations and appropriate interventions to mitigate them, equitable and widespread implementation of proven interventions to increase health equity, such as equitable access to care and preventive measures, can help reduce health disparities.
Farhad Islami
This is one of the few studies that look at the link between structural racism and death from a variety of causes. Researchers from the American Cancer Society, led by Farhad Islami, MD, Ph.D., examined county-level data on economic mobility and death from all causes, heart diseases, cerebrovascular diseases, chronic obstructive pulmonary disease (COPD), injury/violence, all malignant cancers, and 14 cancer types in all ages combined, as well as all-cause mortality in people aged 30-39 years. Data for the 30-39 year age group covered 69 percent of individuals in that age group nationally, and data for all ages combined covered 82 percent to 90 percent of the U.S. population.
The researchers compared four demographic groups: white men, Black men, white women, and Black women. They examined administrative data on upward mobility, such as tax records and mortality statistics, from 3,030 U.S. counties for people born between 1978 and 1983, totaling more than 40 million people. The cohort was followed up on until 2017, when the oldest members were 39 years old.
The analysis found that, with the exception of white males, early life barriers to upward mobility closely predict higher chances of death in early adulthood, with Black males having the strongest association. Additional analyzes that took into account education levels and the types of places people live revealed that the relationship between upward mobility and early-adult mortality is strongest among Black males without college degrees and those who live in cities.

“While more research is needed to identify factors mediating these associations and appropriate interventions to mitigate them,” said Dr. Islami, “equitable and widespread implementation of proven interventions to increase health equity, such as equitable access to care and preventive measures, can help reduce health disparities.”
Death rates in the United States are higher among non-Hispanic Black (Black) people than among non-Hispanic White (White) people, according to the findings. Based on data from 471 counties, a one percentile increase in the economic mobility gap was associated with a 6.8 percent increase in the Black-White mortality gap among males and a 10.7 percent increase in the Black-White mortality gap among females aged 30-39 years.
Based on data from 1,572 counties, the corresponding percentages for males were 10.2 percent and 14.8 percent for females, equating to an increase in the mortality gap of 18.4 and 14.0 deaths per 100,000, respectively. Similarly, for major causes of death, such as COPD, injury/violence, and cancers of the lung, liver, and cervix, strong associations between the economic mobility gap and mortality gap were found at all ages.
“Dismantling structural racism will necessitate increased efforts to implement meaningful institutional changes, as well as broad societal engagement to create equitable local, state, and federal policies,” the authors write. “The findings of this study could help advocate for and inform public policies to improve equity, as well as establish a benchmark for measuring progress in reducing structural racism and its negative health effects.”
According to one of the first studies to put a number on how much of the divide can be attributed to disparities in socioeconomic characteristics, differences in factors such as income, education, and marital status may contribute overwhelmingly to the gap in life expectancy between blacks and whites in the United States.