A research team lead by Albert Einstein College of Medicine experts has found a novel and extremely promising technique for overcoming a major cause of cancer deaths: cancer cells’ ability to thrive in the face of chemotherapy treatments designed to eliminate them.
The researchers utilized a two-drug combination to achieve the purpose of chemotherapy: to cause cancer cells to self-destruct via the biological process known as apoptosis, also known as programmed cell death, as published in the issue of Nature Communications. The treatment was effective against human cancer cell lines that resisted apoptosis while being exposed to several types of chemotherapy, as well as apoptosis-resistant human tumors implanted in mice (i.e., xenograft mouse models).
“Targeted therapies that focus on specific genetic vulnerabilities of cancers have vastly improved treatment in recent years, but not everyone has benefited,” said Evripidis Gavathiotis, Ph.D., Einstein professor of biochemistry and medicine, co-leader of the Cancer Therapeutics Program at the NCI-designated Albert Einstein Cancer Center, and the paper’s corresponding author. “We need new, broadly active medications that can tackle a variety of tumors with fewer side effects than present treatments, and we believe that our novel therapeutic technique will prove to be a viable choice.”
Targeted therapies that focus on specific genetic vulnerabilities of cancers have vastly improved treatment in recent years, but not everyone has benefited. We need new, broadly active medications that can tackle a variety of tumors with fewer side effects than present treatments, and we believe that our novel therapeutic technique will prove to be a viable choice.
Evripidis Gavathiotis
Eliminating Unwanted Cells
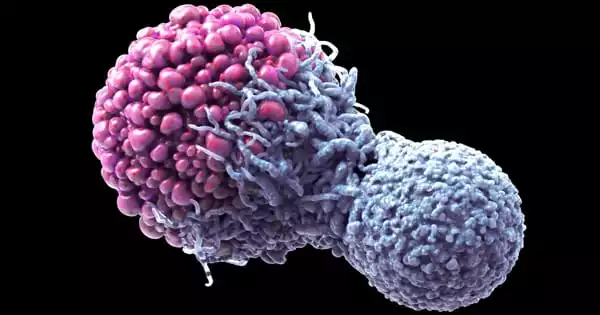
Apoptosis is used by the body to get rid of undesired cells, such as extra cells trimmed during embryological development and damaged cells that need to be destroyed so they don’t survive to develop into cancer cells. Chemotherapy and radiation both rely on severely harming cancer cells in order for them to undergo apoptosis – which, sadly, does not always occur.
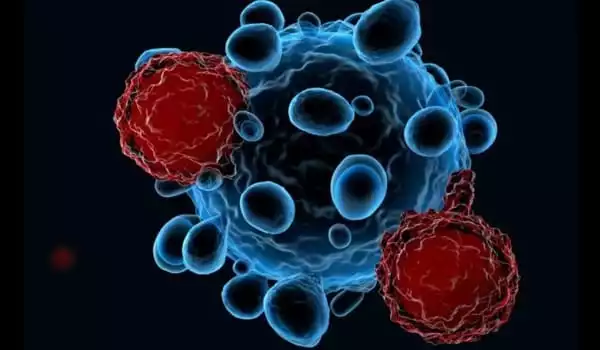
Every cell in the body bears the seeds of its own demise: roughly two dozen apoptotic proteins that perform a life-or-death balancing act. Some proteins promote apoptosis (pro-apoptotic proteins), whereas others inhibit it (anti-apoptotic proteins). For example, DNA damage shifts the balance in favor of cell death, causing the cell to express and activate pro-apoptotic proteins that eventually destroy the cell by poking holes in its mitochondria. Dr. Gavathiotis and colleagues’ new medicine combination kills apoptosis-resistant cancer cells by increasing the active form of one pro-apoptotic protein in particular: BAX, dubbed the “executioner protein.”
Enhancing the “Executioner Protein”
Dr. Gavathiotis identified the first tiny, human-made chemical capable of directly activating BAX in 2012. In their new study, he and his colleagues tested whether BTSA1.2, their third-generation BAX activator, would be effective against a diverse group of 46 human blood and solid tumor cell lines, including non-small cell lung cancer, breast, colorectal, pancreatic, melanoma, leukemia, and lymphoma cell lines. Most of the cell lines had previously resisted all pro-apoptotic medicines discovered.
BTSA1.2 did not perform well against a variety of solid tumor cell lines. The issue was that while BTSA1.2 was raising levels of active pro-apoptotic BAX in solid tumor cells, an anti-apoptotic protein called BCL-XL was neutralizing BAX. The researchers then created a novel technique for eliminating apoptosis-resistant cancer cells: combine BAX-boosting BTSA1.2 with Navitoclax, an investigational pro-apoptotic cancer medication that inhibits BCL-XL.
The combination of BTSA1.2 and Navitoclax proved to be a game-changer. When Dr. Gavathiotis and colleagues, led by co-first author Andrea Lopez, Ph.D., tested the drug duo against the 46 cell lines, it delivered a one-two punch, with BTSA1.2 boosting active BAX to toxic levels in cancer cells and Navitoclax acting as BAX’s bodyguard by preventing BCL-XL from neutralizing BAX.
Limiting Side Effects
The two orally administered medicines were next evaluated against apoptosis-resistant tumor xenografts, in this case, mice implanted with tumor cells from a colorectal-cancer cell line that had resisted BTSA1.2 and Navitoclax alone but succumbed to their combined use. The in vivo investigation yielded comparable results: mice were treated with BTSA1.2, Navitoclax, or the two medicines together once xenografts were developed. Individually, each treatment had limited impact in suppressing tumor growth, but when combined, tumor growth was dramatically decreased, demonstrating that the two drugs work synergistically to fight apoptosis-resistant malignancies.
“Most importantly, mice given the two-drug combination tolerated it exceptionally well,” Dr. Gavathiotis said. “Moreover, research of the treated mice revealed that the two-drug combination had no effect on healthy cells, possibly making it safer than current chemotherapies, which are hazardous to all dividing cells, malignant and normal.”