Parkinson’s disease is often diagnosed using a combination of clinical examination, medical history, and imaging tests such as an MRI or DaTscan. Researchers are constantly attempting to develop more accurate and accessible diagnostic procedures, such as blood tests and biomarkers, but I am unaware of any recent advancements in this field.
Researchers have developed a blood test that detects Parkinson’s disease, potentially paving the path for earlier diagnosis of the disorder.
A new blood-based diagnostic test would be a significant step forward for Parkinson’s disease, which affects 10 million people globally and is the second-most common neurological disease after Alzheimer’s. The study, led by a team of Duke Health neuroscientists, was published on August 30 in the journal Science Translational Medicine.
“Currently, Parkinson’s disease is largely diagnosed based on clinical symptoms after significant neurological damage has already occurred,” said senior author Laurie Sanders, Ph.D., an associate professor in the departments of Neurology and Pathology at Duke University School of Medicine and a member of the Duke Center for Neurodegeneration and Neurotherapeutics.
Our hope is that this assay could not only diagnose Parkinson’s disease, but also identify drugs that reverse or halt mitochondrial DNA damage and the disease process. This disease wreaks havoc on people, and we’re still only treating the symptoms.
Laurie Sanders
“A simple blood test would allow us to diagnose the disease earlier and start therapies sooner,” Sanders went on to say. “Additionally, a clear-cut diagnosis would accurately identify patients who could participate in drug studies, leading to the development of better treatments and potentially even cures.”
Sanders and colleagues focused on DNA damage in the mitochondria as a biomarker for their diagnostic tool. Mitochondria are factories within cells that turn raw energy into usable energy. They have their own DNA, which can be damaged independently of the nuclear DNA, which encodes the majority of an organism’s genome.
Previous research has linked mitochondrial DNA damage to an increased risk of Parkinson’s disease, and the Duke-led team previously observed an accumulation of mitochondrial DNA damage in the brain tissue of deceased Parkinson’s patients.
The Duke researchers used polymerase chain reaction (PCR) technology to build an assay that correctly assessed increased amounts of mitochondrial DNA damage in blood cells obtained from Parkinson’s disease patients compared to persons without the disease.
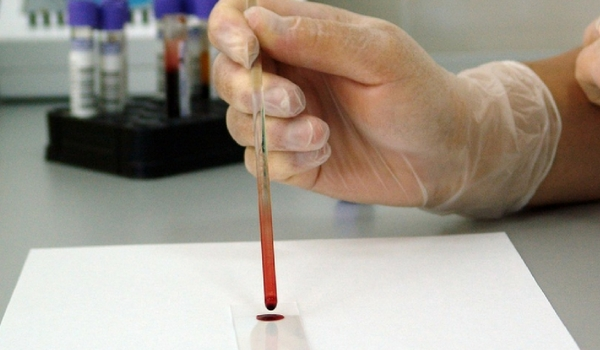
The new test also identified high levels of the damaged DNA in the blood samples of people who harbor the genetic mutation LRRK2, which has been associated with an increased risk of the disease. The assay was able to detect patients with Parkinson’s disease with and without LRRK2 mutations.
A further study in cells from Parkinson’s disease patients looked at whether the team’s PCR-based test could predict the efficacy of a therapy that targets the consequences associated with LRRK2 mutation.
The test found decreased mitochondrial DNA damage in cells treated with an LRRK2 inhibitor compared to samples from patients who did not receive the inhibitor in these samples. This shows that the assay could assist in identifying Parkinson’s disease patients who may benefit from LRRK2 kinase inhibitor therapy even if they do not have an LRRK2 mutation.
“Our hope is that this assay could not only diagnose Parkinson’s disease, but also identify drugs that reverse or halt mitochondrial DNA damage and the disease process,” Sanders said in a statement. “This disease wreaks havoc on people, and we’re still only treating the symptoms.” It’s critical to get novel, effective therapies to market.”
Sanders stated that the research team’s next plans include evaluating the assay in samples from patients in the early stages of disease, before symptoms appear.